Magnesium for Women’s Hormones
Most women don’t realize that their symptoms of hormonal imbalance could be due to low magnesium. Even if you don’t have magnesium deficiency, only suboptimal levels, it can contribute to your symptoms.
Day-to-day symptoms of low magnesium are often vague. This is why most doctors don’t even think to test for magnesium. But magnesium insufficiency is more common than you may think. It’s estimated that two-thirds of the population in the Western world and 68% of Americans don’t get their recommended daily intake for magnesium.
Low magnesium can affect your thyroid hormones, pancreatic hormones, and sex hormones.
If you want to find out whether your magnesium status is contributing to your hormonal symptoms or not, you should use tests that reflect whole-body magnesium. That way, you can ensure you’re getting enough magnesium with extra supplementation.
Let’s delve a little more into how magnesium can help to balance your hormones.

How Magnesium Helps with Women’s Hormones
Magnesium and Hormone Balance
Magnesium helps to regulate various hormones including:
- Insulin
- Thyroid hormones
- Sex hormones estrogen, progesterone, and testosterone
- Cortisol
Insulin
Insulin is a hormone released by your pancreas in response to sugar in your bloodstream. Magnesium controls the release of insulin and helps to regulate your blood sugar. It plays an important role in keeping your body sensitive to insulin and preventing insulin resistance.
A systematic review concluded that magnesium supplementation for more than 4 months improved insulin sensitivity and fasting glucose levels in both healthy and unhealthy subjects.
Thyroid Hormones
Magnesium is required to convert the inactive thyroid hormone (T4) into its active form (T3). If your body can’t make this conversion, your thyroid will not function properly. T3 impacts every cell and organ in your body.
Sex Hormones
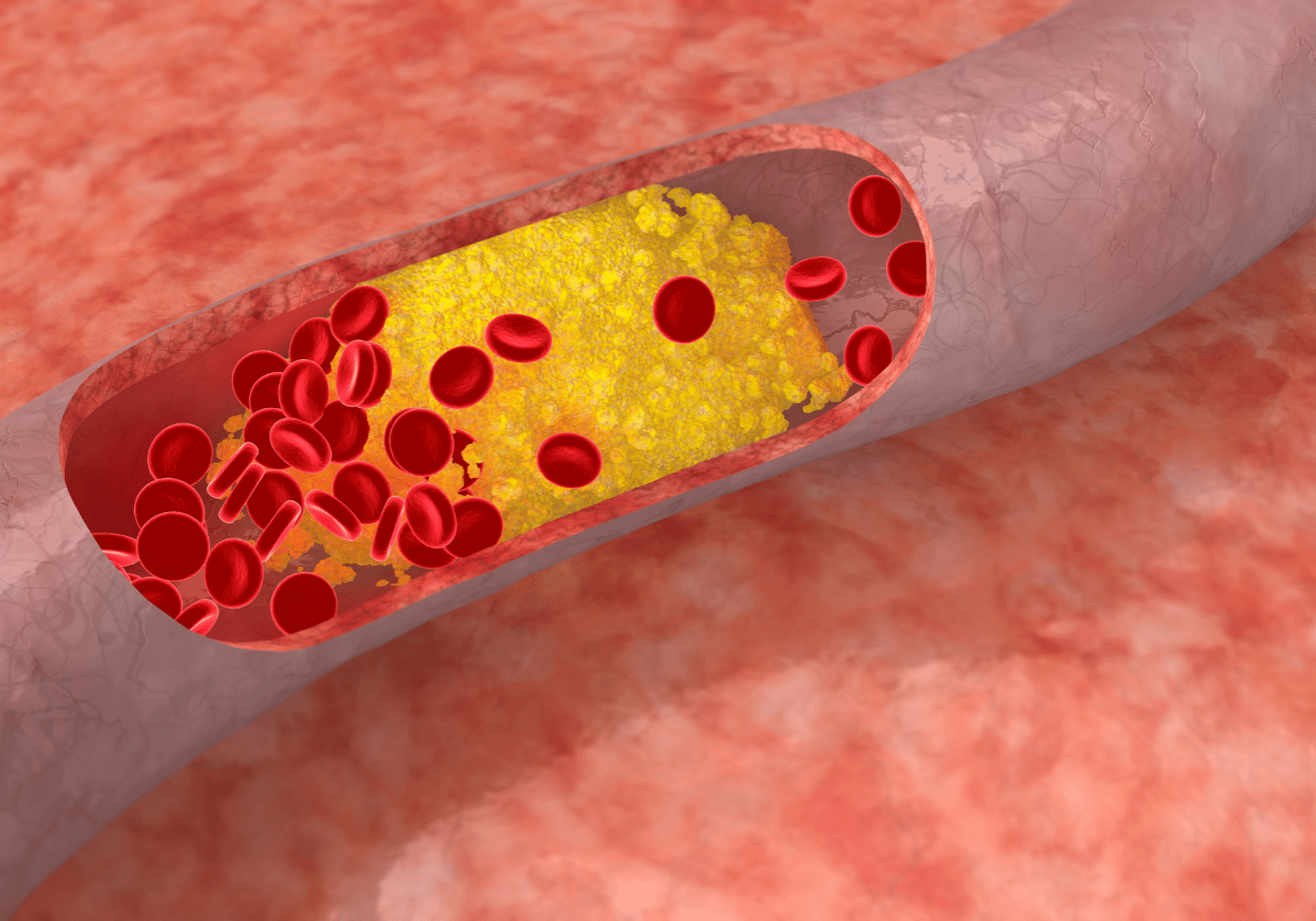
Magnesium plays a crucial role in the production of your steroid hormones (estrogen, progesterone, and testosterone) and adrenal gland hormones (cortisol and aldosterone). It does this through its role in cholesterol metabolism, enzymatic reactions, and hormone receptor functions.
Cholesterol is a precursor to all your steroid hormones. Magnesium helps to metabolize cholesterol into pregnenolone.
Many of the more than 300 enzymatic reactions that magnesium is involved in are related to the synthesis of your steroid hormones. Also, magnesium helps to activate hormone receptors and allows the binding of steroid hormones to their receptors.
Cortisol
Magnesium has a calming effect. It modulates the stress response, levels of GABA, and cortisol.
As previously discussed, magnesium plays a role in the production of all steroid hormones including cortisol from the adrenal glands. It also aids in breaking down cortisol and mitigates the effects of other stress hormones once the stressful events pass.
In a study, forty-nine overweight men and women, aged between 45 and 70 years, took 350mg/day of magnesium for 24 weeks. Compared to the placebo group, those in the magnesium group had less urinary cortisol excretion after the 6 month trial period.
Both subjective stress levels and objective cortisol levels are associated with magnesium status in the body.
In addition, magnesium can help to relax muscles, aid sleep quality, and many other factors related to stress.
Magnesium and PMS

Many women think PMS is normal because it’s so common. However, magnesium deficiency is also common and can clearly make PMS symptoms worse.
Studies have found that women with PMS have lower magnesium levels in red blood cells (RBCs) and white blood cells (WBCs) than women without PMS. Compared to healthy women (n=19), 26 women with PMS had significantly lower RBC magnesium throughout their whole menstrual cycle.
Thus, a question arises whether increasing magnesium levels can improve PMS symptoms.
A pilot study was done to answer this question. Forty-one women aged 18-50 years old with PMS took 250mg of modified-release magnesium over 3 menstrual cycles. They took the magnesium only in the second half of their cycles. After 3 months of supplementation, PMS symptoms improved.
A double-blinded and placebo-controlled clinical trial compared the effectiveness of magnesium, a combination of magnesium and vitamin B6, and a placebo, on the severity of PMS symptoms in women aged 15-45 years old. 50 subjects were assigned to each group.
They found that the group that took a combination of 250mg of magnesium and 40mg of vitamin B6 daily for 4 months had the greatest decrease in PMS symptoms, compared to the other two groups.
Specific symptoms of PMS can include cramps, headaches, mood swings, and more. Magnesium relaxes the smooth muscles of the uterus and reduces prostaglandins that cause discomfort.
In another double-blind and placebo-controlled study, 20 patients with menstrual migraine were treated with 360mg of magnesium pyrrolidone carboxylic acid for 2 months. At baseline, intracellular magnesium levels in women with menstrual headaches were lower than in healthy women.
With magnesium supplements, magnesium levels significantly increased in only their white blood cells. Interestingly, magnesium levels didn’t change much in plasma or red blood cells.
Magnesium can also have an effect on your mood. Magnesium has a calming effect through its interaction with GABA receptors. GABA is an inhibitory neurotransmitter that promotes relaxation. Magnesium can also impact the balance of other neurotransmitters such as serotonin by modulating NMDA receptors. NMDA receptors are involved in neurotransmitter release.
Although it is not a cure-all, magnesium is a simple mineral that can help alleviate PMS symptoms for most premenopausal women. And taking magnesium along with other cofactors such as vitamin B6 improves outcomes even more.
Magnesium and Menopause

Just as magnesium can help premenopausal women, it can help women in menopause as well. Some of the more common symptoms that you could experience during menopause include hot flashes and declining bone density.
A low level of estrogen is a normal part of the aging process and a natural consequence of menopause. It can lead to menopausal symptoms such as hot flashes, night sweats, and vaginal dryness in some women at varying degrees. But it’s important to note that not all women experience these symptoms.
Having a low level of estrogen is not necessarily bad. There is no evidence that women with low estrogen fare worse than those with higher estrogen.
Interpreting serum magnesium can be tricky since higher stress levels can increase serum magnesium and magnesium excretion, while you’re losing whole-body magnesium.
Serum magnesium is not an indicator of whole-body magnesium status. In many cases, high serum magnesium means supplementing with magnesium is beneficial. Therefore, assessing magnesium status should take into account tests for magnesium inside cells along with symptoms and history.
A controlled clinical study compared the levels of sex steroid hormones and serum magnesium in healthy women in 2 different groups (child-bearing age vs. menopause). The outcome was that serum magnesium was inversely related to estrogen levels in postmenopausal women. The lower the estrogen, the higher their serum magnesium was.
Similarly, pregnant women and menopausal women that are treated with hormone replacement therapy, who have relatively higher estrogen, have decreased serum magnesium.
A clinical study found that supplementation of 400mg/day of magnesium (increasing to 800mg/day if needed) for four weeks reduced the severity and frequency of hot flashes in 20 women. The authors postulated that the supplemental magnesium may have made the blood vessels more stable and less sensitive to hormone changes, thus reducing hot flashes.
Magnesium is important for bone health as approximately 60% of magnesium is stored in your bones. Consuming enough magnesium is crucial for mitigating age-related bone loss. When estrogen levels rapidly drop during menopause, osteoclasts, the cells that break down your bones, become more active.
In rats with induced magnesium deprivation., the magnesium deficiency led to:
- Bone loss
- Decrease in osteoblasts (bone-building cells)
- Increase in osteoclasts (cells that break down bone)
- Low serum parathyroid hormone (PTH) and vitamin D levels, which are important for bone health.
Best Magnesium for Hormone Balance

When you supplement with magnesium to improve your hormone balance, taking the right forms will be key to increasing your intracellular magnesium. This is where magnesium does the majority of its important work for its various biochemical reactions.
Less than one percent of the total body magnesium is in your serum. Your body tries to maintain a fairly normal level of serum magnesium despite magnesium deficiency. Therefore, serum magnesium level is not the best marker of magnesium status in the body.
On the other hand, magnesium inside cells such as RBC magnesium is more likely to reflect your total magnesium status.
Although there are many forms of magnesium supplements you can take, not all of them increase RBC magnesium efficiently. For example, although magnesium oxide is the best studied, it’s poorly absorbed.
Chelated magnesium is bound to another organic compound or amino acid (such as magnesium citrate and magnesium glycinate), while non-chelated magnesium includes magnesium oxide and magnesium sulfate.
In general, chelated minerals have higher bioavailability and are better absorbed through the small intestine into the bloodstream.
Animal studies have also demonstrated that different organic forms deliver magnesium to different tissues. For example, in rats, magnesium malate delivers the most to muscles, whereas magnesium acetyl taurate delivers the most to the brain.
Therefore, many nutritionists and expert clinicians believe it’s best to take a combination of various forms of magnesium instead of just one.
Sucrosomial magnesium is the newest form of magnesium that is highly bioavailable. It uses sucrose esters of fatty acids to deliver magnesium for better solubility, absorption, and bioavailability.
Ten healthy subjects randomly took 350mg of four different types of magnesium (sucrosomial magnesium, magnesium oxide, magnesium citrate, and magnesium bisglycinate). After one dose, the Sucrosomial magnesium resulted in the fastest absorption and highest bioavailability of all the other forms of magnesium at 24 hours.
Based on the above information, the best magnesium supplement for hormone balance should include Sucrosomial magnesium. In addition, it should include a combination of various forms of magnesium to target different tissues. And even better, if it includes the cofactors, the effectiveness of magnesium will be boosted.
Biooptimizer’s Magnesium Breakthrough is a product that delivers all these ingredients. It provides the 7 best-absorbed forms of magnesium in a humic/fulvic blend along with cofactors vitamin B6 and manganese. It is the perfect magnesium supplement to support your hormone balance.
Conclusion
If you are currently experiencing PMS symptoms or menopausal symptoms, you may benefit from supplementing with extra magnesium. Low levels of magnesium are more common than you may think and could be contributing to your hormonal symptoms.
Since it’s not always easy to meet the daily minimum, supplementing with magnesium will be the next best method for ensuring you have optimal levels of magnesium.
- Schwalfenberg GK, Genuis SJ. The importance of magnesium in clinical healthcare. Scientifica (Cairo). 2017;2017:4179326. doi:10.1155/2017/4179326
- Simental-Mendía LE, Sahebkar A, Rodríguez-Morán M, Guerrero-Romero F. A systematic review and meta-analysis of randomized controlled trials on the effects of magnesium supplementation on insulin sensitivity and glucose control. Pharmacol Res. 2016;111:272-282. doi:10.1016/j.phrs.2016.06.019
- Boyle NB, Lawton C, Dye L. The effects of magnesium supplementation on subjective anxiety and stress-A systematic review. Nutrients. 2017;9(5). doi:10.3390/nu9050429
- Pickering G, Mazur A, Trousselard M, et al. Magnesium status and stress: The vicious circle concept revisited. Nutrients. 2020;12(12):3672. doi:10.3390/nu12123672
- Schutten JC, Joris PJ, Minović I, et al. Long-term magnesium supplementation improves glucocorticoid metabolism: A post-hoc analysis of an intervention trial. Clin Endocrinol (Oxf). 2021;94(2):150-157. doi:10.1111/cen.14350
- Cuciureanu MD, Vink R. Magnesium and Stress. University of Adelaide Press; 2011.
- Rosenstein DL, Elin RJ, Hosseini JM, Grover G, Rubinow DR. Magnesium measures across the menstrual cycle in premenstrual syndrome. Biol Psychiatry. 1994;35(8):557-561. doi:10.1016/0006-3223(94)90103-1
- Quaranta S, Buscaglia MA, Meroni MG, Colombo E, Cella S. Pilot study of the efficacy and safety of a modified-release magnesium 250mg tablet (sincromag??) for the treatment of premenstrual syndrome. Clin Drug Investig. 2007;27(1):51-58. doi:10.2165/00044011-200727010-00004
- Fathizadeh N, Ebrahimi E, Valiani M, Tavakoli N, Yar MH. Evaluating the effect of magnesium and magnesium plus vitamin B6 supplement on the severity of premenstrual syndrome. Iran J Nurs Midwifery Res. 2010;15(Suppl 1):401-405.
- Facchinetti F, Sances G, Borella P, Genazzani AR, Nappi G. Magnesium prophylaxis of menstrual migraine: Effects on intracellular magnesium. Headache. 1991;31(5):298-301. doi:10.1111/j.1526-4610.1991.hed3105298.x
- Muneyyirci-Delale O, Nacharaju VL, Dalloul M, Altura BM, Altura BT. Serum ionized magnesium and calcium in women after menopause: inverse relation of estrogen with ionized magnesium. Fertil Steril. 1999;71(5):869-872. doi:10.1016/s0015-0282(99)00065-5
- Stanton MF, Lowenstein FW. Serum magnesium in women during pregnancy, while taking contraceptives, and after menopause. J Am Coll Nutr. 1987;6(4):313-319. doi:10.1080/07315724.1987.10720193
- Murray MT. Magnesium supplementation reduces hot flashes in women with breast cancer. Naturalmedicinejournal.com. Published March 23, 2014. Accessed July 20, 2023. https://www.naturalmedicinejournal.com/journal/magnesium-supplementation-reduces-hot-flashes-women-breast-cancer
- Castiglioni S, Cazzaniga A, Albisetti W, Maier JAM. Magnesium and osteoporosis: current state of knowledge and future research directions. Nutrients. 2013;5(8):3022-3033. doi:10.3390/nu5083022
- Rude RK, Singer FR, Gruber HE. Skeletal and hormonal effects of magnesium deficiency. J Am Coll Nutr. 2009;28(2):131-141. doi:10.1080/07315724.2009.10719764
- Uysal N, Kizildag S, Yuce Z, et al. Timeline (bioavailability) of magnesium compounds in hours: Which magnesium compound works best? Biol Trace Elem Res. 2019;187(1):128-136. doi:10.1007/s12011-018-1351-9
- Brilli E, Khadge S, Fabiano A, et al. Magnesium bioavailability after administration of sucrosomial magnesium: results of an study and a comparative, double-blinded, cross-over study in healthy subjects. Europeanreview.org.






