Part 2: Best Tests For Whole-Body Magnesium Deficiency And Statuses: Accuracies, Pros, And Cons

In this part you will discover the invaluable insights offered by the magnesium tests available.
In the last article, part 1, we covered:
- Why low serum magnesium levels are very different from low whole-body magnesium
- Why it’s hard to accurately test for whole body magnesium
In this article, part 2, we’ll cover all commercially available tests and reasonable ways to assess magnesium levels, along with:
- How accurately each of these tests reflect whole-body magnesium levels
- Their pros and cons
- References and normal ranges
Best Magnesium Tests: How They Work, Accuracy Levels, Optimal Ranges, Pros, And Cons
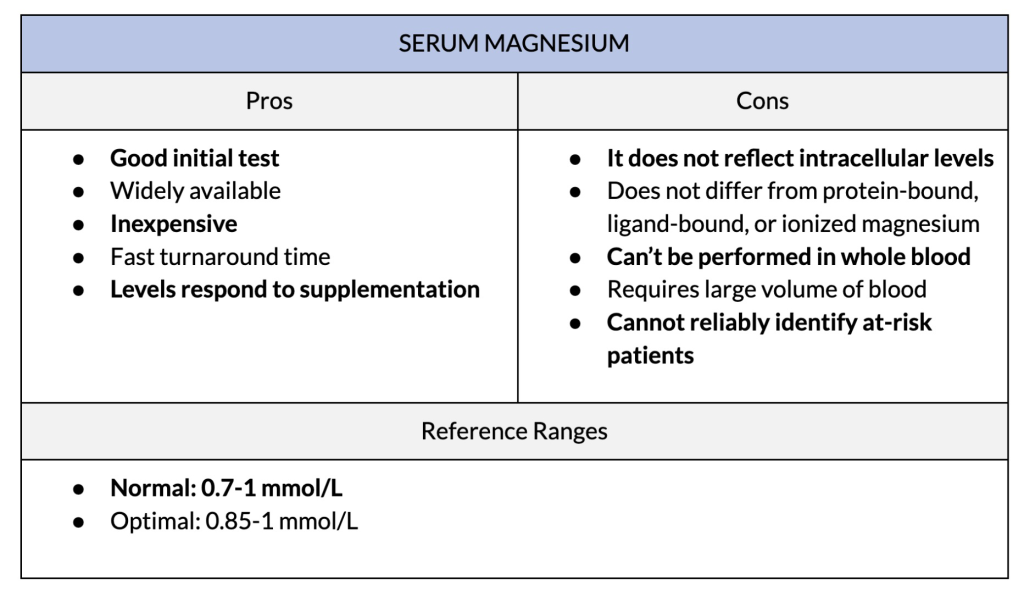
1. Serum Magnesium

The term “magnesium blood test” typically refers to serum magnesium, but can sometimes refer to whole blood magnesium.
Serum magnesium is the most common initial magnesium test. It measures the concentration of magnesium in the water portion of your blood. However, since only 1% of your body’s magnesium lies in the blood, and 0.3% in the serum, the serum test doesn’t reflect whole-body magnesium.
You can have normal or even high serum magnesium, even while your whole body is low in or losing magnesium. For example, stress can raise serum magnesium, but it causes your entire body to lose magnesium. In fact, among ICU patients, high-normal serum magnesium predicts deaths in the hospital.
Serum levels can also be affected by many things, including:
- Time of the day that you draw the blood
- The amount of albumin in the blood
- Kidney filtration
- And more
If you’ve just taken a magnesium supplement, your serum magnesium levels will increase. However, this doesn’t necessarily mean you’ve corrected a magnesium deficiency. You want the type of magnesium supplement that goes inside your cells.
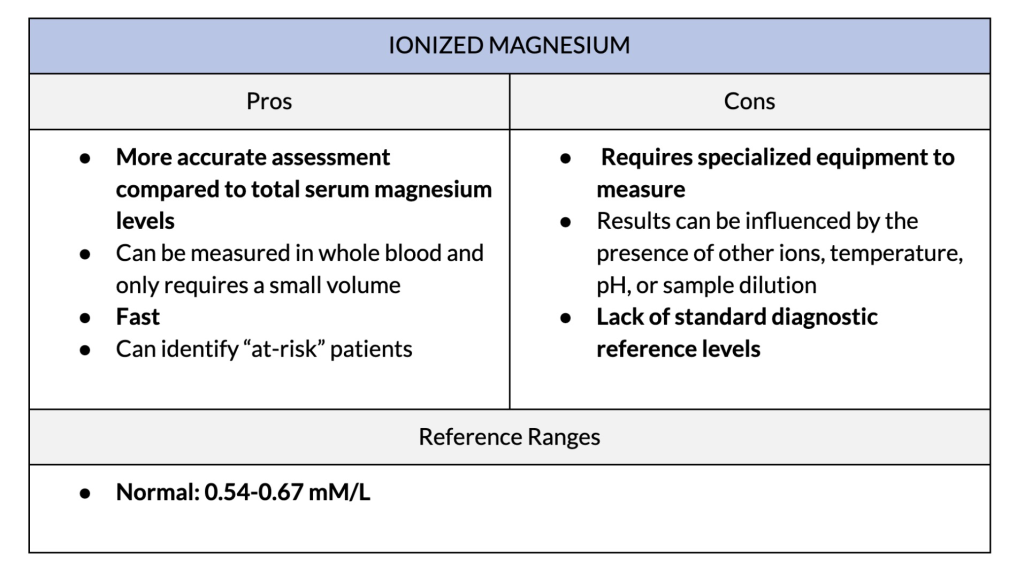
2. Ionized Magnesium
Ionized magnesium is the free, biologically active fraction of magnesium in the blood. It is a more sensitive indicator of how much magnesium is available at the cellular level. This test is often used to diagnose critically ill patients with magnesium deficiency.
Ionized magnesium plays an important role in maintaining homeostasis in the body, and generally represents 55-70% of extracellular magnesium. It is difficult to calculate, which is why it is a test that is not often conducted.
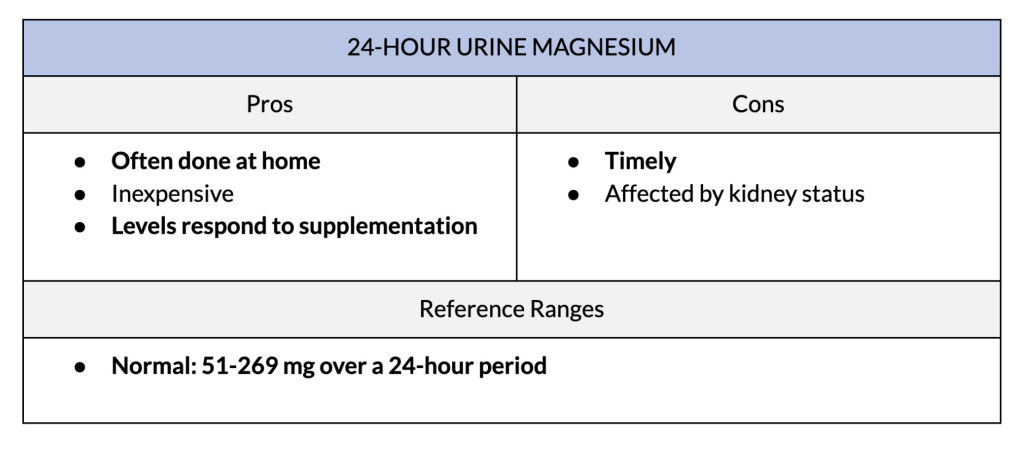
3. 24-Hour Urine Magnesium Test
The 24-hour urine magnesium test measures how much magnesium is excreted in urine over a one-day period. It is helpful in evaluating overall magnesium status and may provide a more comprehensive assessment compared to blood tests.
The test measures magnesium in your urine samples over a 24-hour period. This methos can provide a better understanding of magnesium balance. It can also monitor your response to magnesium supplementation and how well your kidneys handle the supplement.

The laboratory determines how much magnesium you urinate out by multiplying the magnesium concentration by your total urine volume. The result provides the amount excreted in a given timeframe. The values then can be compared to reference ranges or previous measurements to assess magnesium balance.
Lower levels of urinary magnesium excretion may suggest magnesium deficiency, while higher levels may indicate excess magnesium or impaired kidney function. However, urine magnesium levels may not acutely reflect magnesium levels in the body, as results are dependent on how much the kidneys are filtering or absorbing. There is also a poor correlation between serum magnesium levels and urinary magnesium levels.
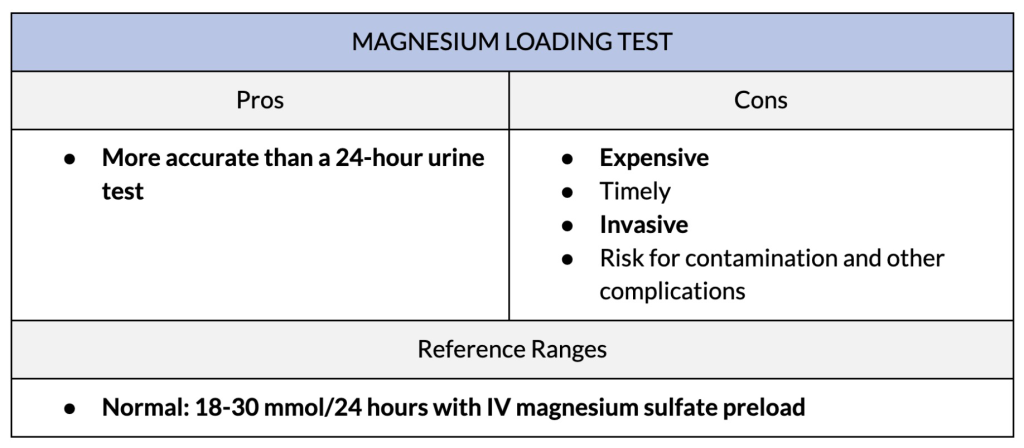
4. Magnesium Loading Challenge
Another way to assess magnesium status is with a magnesium loading challenge. This test is helpful to understand how the body utilizes and retains magnesium. The loading challenge can also be used to monitor your response to magnesium supplements, or to assess how well supplementation works for certain conditions when deficiency is common or suspected.
This test involves administering a controlled dose of magnesium, typically intravenously (through an IV). By administering magnesium this way, it bypasses the normal digestive processes and allows it to be directly delivered to the bloodstream.
Once the magnesium solution is administered, the health provider administering the test will monitor how much magnesium is excreted in your urine over a specific period. This period is usually over 24 hours. One specific test, called Thoren’s intravenous magnesium load, is conducted over 16 hours.

Results are interpreted by comparing the amount of magnesium administered to the amount excreted in the urine. If the excretion of magnesium is much higher than expected, it suggests the body has difficulty retaining or using magnesium effectively and indicates a deficiency.
Thoren’s magnesium load test is interpreted slightly differently. His work suggests that if less than 70% of IV magnesium is given over 16 hours, magnesium deficiency is likely. This is because the body is trying to take up as much magnesium as possible, so less is excreted in the urine. This method should be used in combination with other magnesium markers but indicates that high magnesium uptake means deficiency is likely even when blood levels are normal.
Both tests are particularly helpful when there is a suspected deficiency, but other laboratory results are unclear. However, both tests require supervision under a healthcare provider and urinary measurements to be accurate, which can pose challenges when trying to interpret results. It also tends to be expensive.
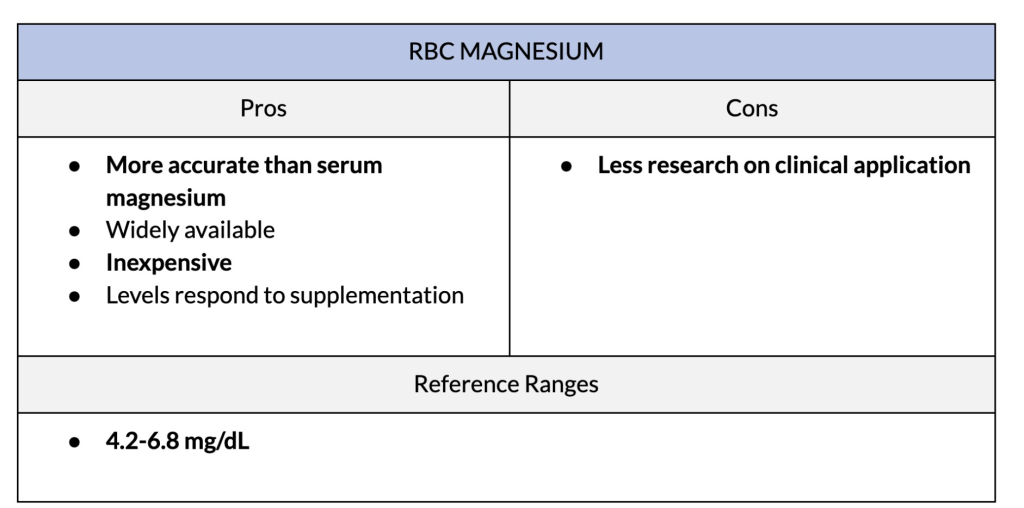
5. Red Blood Cell Magnesium
Red blood cell magnesium (RBC magnesium) measures the amount of magnesium found within red blood cells. It differs from serum magnesium testing in the compartment of blood that is being evaluated. Compared to serum magnesium, which measures the magnesium concentration in the liquid portion of the blood, RBC magnesium measures magnesium levels within RBCs themselves.
RBC magnesium is a more accurate reflection of magnesium inside your cells because red blood cells contain a significant portion of the body’s magnesium content. Red blood cells contain proteins that move magnesium in and out of cells. This helps to maintain a balance between intracellular and extracellular magnesium levels.
This is one of the reasons we created Magnesium Breakthrough with forms of magnesium that have been proven to increase red blood cell magnesium.
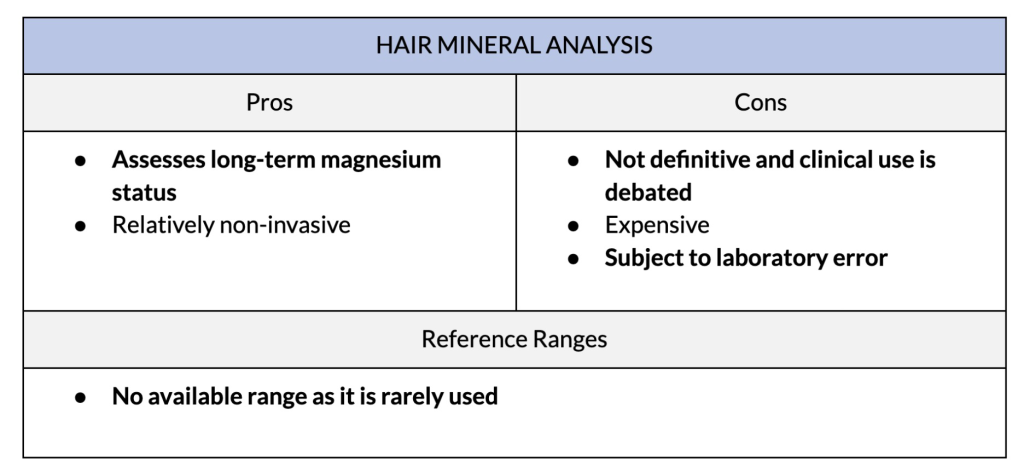
6. Hair Mineral Analysis
Minerals, including magnesium, are incorporated into your hair as it grows and has been thought to reflect body levels. The hair mineral analysis test is done by sampling a portion of hair that has been cut adjacent to the scalp using sterile scissors. The hair is then analyzed in a lab for its mineral content.
Compared to blood and urine tests, which reveal the current body state of magnesium, it is thought that hair analysis can help determine what your status has been long term. However, it remains controversial.
This test is not a definitive diagnostic test for magnesium deficiency for several reasons. First, there are many factors that can impact results. These include:
- Hair treatment
- External exposures to magnesium sources
- And variations in the rate of hair growth and loss
There are also differences in how different laboratories interpret results. Finally, the evidence for hair analysis as a true biological marker is lacking.
7. Assessment By Symptoms And Lifestyle Factors
Magnesium deficiency can also be assessed based on symptoms or lifestyle factors that may contribute to poor magnesium status. While not definitive, considering these factors alongside the tests mentioned above can help to identify possible deficiencies.
Some common symptoms of magnesium deficiency include:
- Muscle cramps and spasms: Because of the important role magnesium plays in muscle function, magnesium deficiency can cause muscle cramps, twitches, and spasms. [R19, R9].
- Fatigue and weakness: Low magnesium can increase feelings of weakness and fatigue because of its important role in energy production.
- Irregular heartbeat: Magnesium plays an important role in maintaining a regular heartbeat, and deficiency can result in palpitations or irregular heart rhythms.
- Irritability and reduced stress resilience: Magnesium is involved in regulating neurotransmitters (signaling molecules in the brain). Deficiency may contribute to mood changes and irritability.
- Poor sleep: Low magnesium can disrupt sleep patterns and contribute to poor sleep quality.
- Appetite changes and nausea
- Declining bone density in older populations: It’s normal for bone density to go down over time since hormones that help maintain bone mass, estrogen and testosterone, go down with age. However, since magnesium is a key component of bone tissues, a magnesium deficiency can make this worse.
Some other factors that may contribute to magnesium deficiency include:
- Diet: Eating a diet that is low in magnesium-containing foods ( i.e. leafy greens, nuts, seeds, legumes, and whole grains) may increase the risk of deficiency. A diet lacking carbohydrates and medium-chain fatty acids will increase magnesium uptake, but will also increase the body’s demand as it is involved in pathways to break down these food groups.
- Alcohol: Too much alcohol intake can impair magnesium absorption and increase excretion, which may lead to deficiency
- Medications and health conditions: Certain medications, including diuretics and proton pump inhibitors, can interfere with magnesium absorption. Any health condition that affects the digestive tract or kidneys can also impact magnesium levels.
- Body mass index (BMI): Higher BMI may cause lower magnesium status
- Gender: Estrogen, a hormone that is higher in females, can impact magnesium status. This hormone enhances how magnesium is used in the body and may allow for better magnesium retention.
- Age: Older adults tend to have lower magnesium intake. Changes to the digestive system that occur as you get older can impact how much magnesium your body is able to absorb.
Using symptoms, estimated daily intake, and considering lifestyle factors can help determine your magnesium status. However, a proper assessment should always be conducted with a healthcare provider, as many of the above can be influenced by other factors.
In most cases, since our food chain is low in magnesium and most people don’t get enough from food, it’s best to supplement with a high-bioavailability magnesium supplement to ensure you get enough every day.
- Scarpati G, Baldassarre D, Oliva F, Pascale G, Piazza O. Ionized or Total Magnesium levels, what should we measure in critical ill patients? Transl Med UniSa. 2020;23(4):68-76. doi:10.37825/2239-9747.1015
- Ismail Y, Ismail AA, Ismail AAA. The underestimated problem of using serum magnesium measurements to exclude magnesium deficiency in adults; a health warning is needed for “normal” results. Clin Chem Lab Med. 2010;48(3):323-327. doi:10.1515/CCLM.2010.077
- Jacobsen AA, Bressendorff I, Nordholm A, et al. Diurnal variation of magnesium and the mineral metabolism in patients with chronic kidney disease. Bone Rep. 2021;15(101130):101130. doi:10.1016/j.bonr.2021.101130
- Witkowski M, Hubert J, Mazur A. Methods of assessment of magnesium status in humans: a systematic review. Magnes Res. 2011;24(4):163-180. doi:10.1684/mrh.2011.0292
- Pickering G, Mazur A, Trousselard M, et al. Magnesium status and stress: The vicious circle concept revisited. Nutrients. 2020;12(12):3672. doi:10.3390/nu12123672
- Tan L, Xu Q, Li C, Liu J, Shi R. High-normal serum magnesium and hypermagnesemia are associated with increased 30-day in-hospital mortality: A retrospective cohort study. Front Cardiovasc Med. 2021;8:625133. doi:10.3389/fcvm.2021.625133
- Radiology management, ICU management, healthcare IT, cardiology management, executive management. Published online 2021. Accessed June 30, 2023. https://healthmanagement.org/c/icu/whitepaper/why-should-we-be-measuring-ionized-magnesium
- Magnesium, 24 hour, urine – mayo clinic laboratories. Testcatalog.org. Accessed June 30, 2023. https://endocrinology.testcatalog.org/show/MAGU
- Workinger JL, Doyle RP, Bortz J. Challenges in the diagnosis of magnesium status. Nutrients. 2018;10(9):1202. doi:10.3390/nu10091202
- Magnesium, Urine, 24 Hour. Uncmedicalcenter.org. Accessed June 30, 2023. https://www.uncmedicalcenter.org/mclendon-clinical-laboratories/available-tests/magnesium-urine-24-hour-/
- Gullestad L, Midtvedt K, Dolva LO, Norseth J, Kjekshus J. The magnesium loading test: reference values in healthy subjects. Scand J Clin Lab Invest. 1994;54(1):23-31. doi:10.3109/00365519409086506
- Sohrevardi SM, Mojtahedzadeh M, Sadray S, et al. Role of magnesium loading test in detecting hypomagnesemia in critically ill patients. Org.br. Accessed June 30, 2023. http://www.bioline.org.br/pdf?mr04006
- Correction: Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Heart. 2018;5(1):e000668corr1. doi:10.1136/openhrt-2017-000668corr1
- 24 hour urine magnesium load test. Allinahealth.org. Accessed June 30, 2023. https://account.allinahealth.org/library/content/49/150513
- Magnesium, RBC. Labcorp. Accessed June 30, 2023. https://www.labcorp.com/tests/080283/magnesium-rbc
- Brilli E, Khadge S, Fabiano A, et al. Magnesium bioavailability after administration of sucrosomial magnesium: results of an study and a comparative, double-blinded, cross-over study in healthy subjects. Europeanreview.org. Accessed June 30, 2023. https://www.europeanreview.org/wp/wp-content/uploads/1843-1851-1.pdf
- Ca mg Na K cu Zn P Fe Mn Cr Se B co mo S Sb U as be Hg Cd Pb Al calcium magnesium sodium potassium copper zinc phosphorus iron manganese chromium selenium boron cobalt molybdeum sulfur antimony uranium arsenic beryllium mercury cadmium lead aluminum. Mineralstate.co.uk. Accessed June 30, 2023. https://www.mineralstate.co.uk/wp-content/uploads/hair-analysis.pdf
- Namkoong S, Hong SP, Kim MH, Park BC. Reliability on intra-laboratory and inter-laboratory data of hair mineral analysis comparing with blood analysis. Ann Dermatol. 2013;25(1):67-72. doi:10.5021/ad.2013.25.1.67
- Magnesium. Nih.gov. Accessed June 30, 2023. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/
- Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Med Hypotheses. 2006;67(2):362-370. doi:10.1016/j.mehy.2006.01.047
- Arab A, Rafie N, Amani R, Shirani F. The role of magnesium in sleep health: A systematic review of available literature. Biol Trace Elem Res. 2023;201(1):121-128. doi:10.1007/s12011-022-03162-1
- Rondanelli M, Faliva MA, Tartara A, et al. An update on magnesium and bone health. Biometals. 2021;34(4):715-736. doi:10.1007/s10534-021-00305-0
- Coudray C, Demigné C, Rayssiguier Y. Effects of dietary fibers on magnesium absorption in animals and humans. J Nutr. 2003;133(1):1-4. doi:10.1093/jn/133.1.1
- Gullestad L, Dolva LO, Søyland E, Manger AT, Falch D, Kjekshus J. Oral magnesium supplementation improves metabolic variables and muscle strength in alcoholics. Alcohol Clin Exp Res. 1992;16(5):986-990. doi:10.1111/j.1530-0277.1992.tb01906.x
- Rivlin RS. Magnesium deficiency and alcohol intake: mechanisms, clinical significance and possible relation to cancer development (a review). J Am Coll Nutr. 1994;13(5):416-423. doi:10.1080/07315724.1994.10718430
- Thongon N. Omeprazole decreases magnesium transport across Caco-2 monolayers. World J Gastroenterol. 2011;17(12):1574. doi:10.3748/wjg.v17.i12.1574
- Thongon N, Krishnamra N. Apical acidity decreases inhibitory effect of omeprazole on Mg(2+) absorption and claudin-7 and -12 expression in Caco-2 monolayers. Exp Mol Med. 2012;44(11):684-693. doi:10.3858/emm.2012.44.11.077
- Swaminathan R. Magnesium metabolism and its disorders. Clin Biochem Rev. 2003;24(2):47-66.
- Rodriguez-Morán M, Guerrero-Romero F. Elevated concentrations of TNF-alpha are related to low serum magnesium levels in obese subjects. Magnes Res. 2004;17(3):189-196. Accessed June 30, 2023.
- De Leeuw I, Vansant G, Van Gaal L. Magnesium and obesity: influence of gender, glucose tolerance, and body fat distribution on circulating magnesium concentrations. Magnes Res. 1992;5(3):183-187. Accessed June 30, 2023. https://pubmed.ncbi.nlm.nih.gov/1467156/
- Ford ES, Mokdad AH. Dietary magnesium intake in a national sample of US adults. J Nutr. 2003;133(9):2879-2882. doi:10.1093/jn/133.9.2879
- Musso CG. Magnesium metabolism in health and disease. Int Urol Nephrol. 2009;41(2):357-362. doi:10.1007/s11255-009-9548-7
2 Comments
Leave a Comment
You must be logged in to post a comment.





Thank you for sharing this comparison. I was particularly interested in the point of view regarding HTMA analysis. Unfortunately, when I looked up the sited references, I am not convinced that your author’s analysis is credible. The first reference (17) is merely a link to a website that describes the HTMA report elements and gives definitions, which is informative, but not relevant to accuracy. The second reference (18) is a study from 2013 in which ONE MAN’s hair samples were tested with different labs lol! The lab names are important….I have been told that some labs wash the hair samples, which makes the sodium and potassium off. I have been told that the most reliable labs for the HTMA test are ARL and Trace Elements. No lab names were given from the 11 year old study that was sited. I have personally seen two tests so far come back from HTMA analysis, and they both seemed in line with the lifestyle that each person. I will be looking at 3 more HTMA results from family/friends, and expect to find credible information. I hope you can update your findings with more current and relevant analysis. I believe this test is more credible that what you describe, based on my personal experience.
Thank you for your feedback, Tina. We searched and couldn’t find many references on this test, even though in our own (and the author’s) clinical experience have found it quite valuable. Do you have any high-quality, credible references on HTMA (ideally scientific and peer-reviewed) that we should check out?
Nattha Wannissorn, PhD, FDN-P, RHN
BiOptimizers Director of Content