How Does Human Genetics Shape the Gut Flora and Microbiome?
How Does Human Genetics Shape the Gut Flora and Microbiome?
From digesting and absorbing nutrients to even regulating your immune system, the microbiome has many influential effects on your overall health and well-being.
While many things can influence the microorganisms living in your gut, new research suggests that specific genetic variations can make people susceptible to having an imbalanced gut microbiome.
Changes in the composition of the gut microbiota may make you more susceptible to leaky gut and intestinal dysbiosis, which can impact digestion, metabolism, and even immunity, as well as many other aspects of health.
Below, we dive deep into the world of genetics and gut health, exploring how genes can influence the composition of your microbiome, the function of your digestive tract, and even your susceptibility to different gut-related disorders.
How does human genetics shape the gut microbiome?
The composition of your microbiome differs from others around you, and gut structure can be partly determined by genetics. However, species of animals that are more closely related tend to have more similar gut microbiomes.
For example, when researchers look at the gut microbes in different types of mammals, they found that despite differences in age, diet, and even where they live, human gut microbes are more alike compared to other species.
Many different factors, genetic and environmental, can influence its composition, including:
- Diet and lifestyle choices which have the biggest impact
- Genetic variations that can influence gut structure, diet preferences, body weight, and immune system activity
- Location and travels
- Whether you were born vaginally or through C-section
- History of antibiotic exposures
Researchers figure out how much of a certain trait can be related to genetics by studying heritability. These may include seeing how many identical twins share the traits, and how the traits run in the family. Heritability data helps scientists understand variations in traits that can be influenced by genes.
Twin studies have discovered that some gut microbiome patterns are partly inherited, Identical twins have more similar gut microbiomes than non-identical twins.
Some genetic variants influence the bacteria strains that take up residence in your gut. Also, these bacteria strains also predict certain heritable traits.
A twin study that looks at common gut bacteria strains in UK twins found Christensenellaceae bacteria, which was linked to lower BMI to be the most heritable. Other heritable microbe strains include Methanobrevibacter and Blautia which point towards genetics impacting a broader range of gut microbes .
Some obesity related genes have been tied to the abundance of specific microbes, including Methanobrevibacter, Christensenellaceae, Blautia, and Akkermansia Researchers believe that genetic variants can impact the gut microbiome and contribute to higher body weights.
Some of the most heritable microbes seem to remain stable over long periods – and therefore less likely to be influenced by things such as diet and lifestyle.
However, these studies in twins also show changes in gut composition over time, cementing the important role that the environment has in shaping the microbiome. Arguably these factors can play an even larger role than genetics in the microbiome!
There are still some genes that can impact your gut health, through a few different mechanisms, and we will break these down below. Note that this is not an exhaustive list as researchers are still identifying more ways that our gut bacteria interact with our gut and genes.
Genes That Affect the Gut Flora
· MUC2
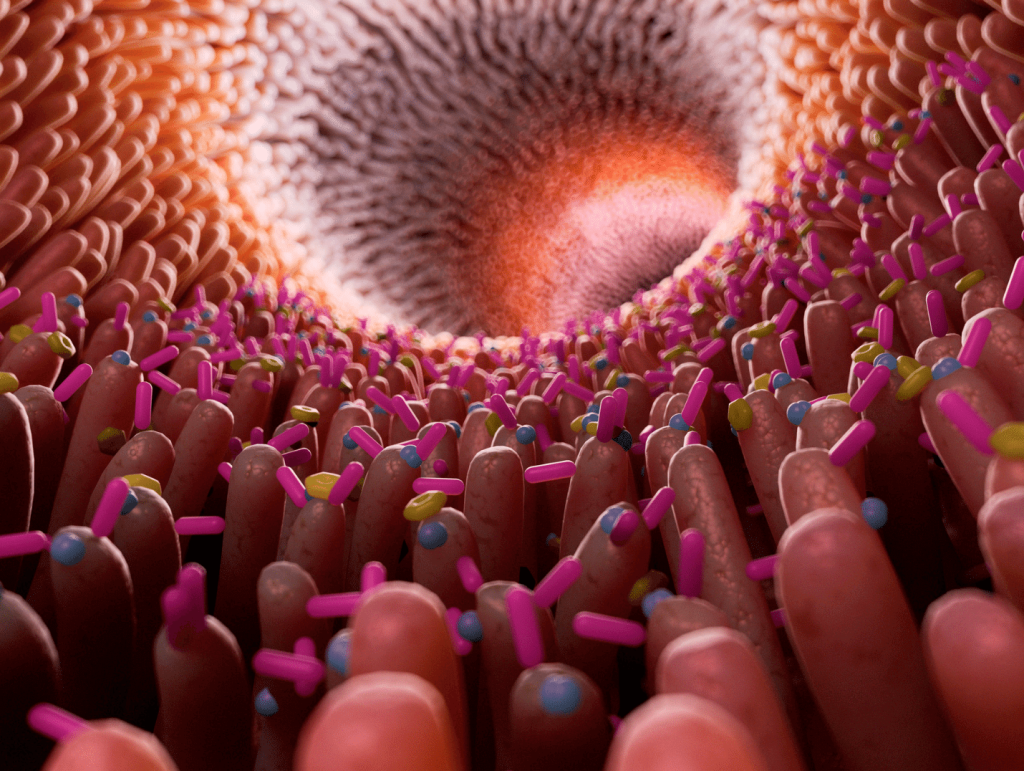
The MUC2 gene encodes a protein called mucin-2, which forms part of the mucus barrier between your microbiome and intestinal lining. Some gut bacteria eat this protective lining as fuel. Parts of mucin-2 also provide nutrients like carbon and nitrogen, which helps fuel good bacteria in your gut.
Researchers uncovered this gene by breeding mice that lack MUC2. The mice went on to develop severe inflammation in their digestive tract because they no longer had a protective mucus lining. This defect led to dysbiosis and disease.
· FUT2
The FUT2 gene encodes a protein called fucosyltransferase 2, which helps synthesize molecules in your digestive tract. Specifically, it plays an important role in attaching fructose (sugar) molecules to the mucin proteins discussed above.
Fructose is an important energy source for certain bacteria and helps them attach to the gut lining and hide from your immune system.
Some variants in FUT2 can prevent good bacteria from colonizing the digestive tract and alter the gut microbiome. This can affect the balance between good and bad microbes. We tend to see fewer good bacteria (such as Bifidobacterium and Bacteroidetes) in those with less functional FUT2 genes, and an overall less robust gut.
· LCT
The LCT gene encodes for the enzyme lactase, which helps your body break down lactose sugars found in dairy products.
Genetic variations in the LCT gene are associated with lactose intolerance. People with LCT gene variants can have reduced lactase activity and develop symptoms of lactose intolerance when they eat dairy products. This can affect how much lactose gut bacteria can ferment.
The good news is that there are other studies that show dietary changes can help. Consuming prebiotic galactans (found in legumes) can help reduce symptoms of lactose intolerance. These molecules can promote the growth of good bacteria that help with lactose digestion and produce less gas and other symptoms.
Can Gut Bacteria Be Inherited?
The first three years of life show rapid changes in flora composition, because of the things you are exposed to in the environment – things you eat, antibiotic exposure, how you were born, and whether you were breastfed or not – all help shape the flora you have as an adult.
Your gut microbiome is first colonized during birth. And the method in which you were born can have a major impact on its composition.
It’s normal for vaginally-delivering mothers to defecate during delivery, and for their babies to swallow their mother’s poop and vaginal fluid. In other words, vaginal delivery exposes the baby to the mother’s vaginal and gut flora, which becomes the initial colonization of your own gut microbiota.
In contrast, if you were born via C-section, you are primarily exposed to skin and environmental bacteria instead of getting it from your mom.
Here are some of the biggest differences:
| Diversity | Composition | Exposure | |
| Vaginal birth | More diverse and richer gut microbiome in early life stages | ·Higher abundance of “good” bacteria, including Bifidobacterium and Lactobacillus, essential for gut and immune health | Direct contact with mother’s vaginal and fecal microbiota, which play important role in initial gut colonization |
| C-Section | Less diversity of gut microbes in early months | Higher abundance of bacteria typically found on the skin, including Staphylococcus and Corynebacterium | No direct exposure to mothers microbiota, which can affect initial gut colonization |
Breast milk is another way that microbes can transmit from mother to baby. Breast milk contains lots of good bacteria, as well as prebiotics, which can help establish a healthy gut. However, the specific microbes found in breast milk can vary between mothers.
Living in close contact with family members can also pass around microbes that make their way to the gut. Families who share the same house tend to have more similar microbiome compositions compared to relatives who live separately.
Therefore, gut flora and microbiomes are naturally inherited.
What Affects the Gut Microbiome Beyond Your Genes?

Besides genetics, there are many other factors that can influence the composition of your gut microbiome. Some of the big players include:
1) Diet
The type of food you eat regularly can directly impact the composition of your microbiome:
- Fiber-rich diets and plant-based foods can promote a diverse and healthy gut microbiome. On the other hand, diets high in processed foods, sugar, and unhealthy fats can negatively impact the gut microbiome.
- Probiotics, the live beneficial bacteria found in fermented foods, also promote gut health. Prebiotics on the other hand, which act as fuel sources for good gut bacteria, can also promote a healthy gut composition.
2) Physical Activity
Physical activity can promote a healthier gut microbiome, promoting microbial diversity and favorable shifts in the microbiome.
Regular exercise has been shown to increase levels of beneficial bacteria Akkermansia and Bacteroides, which are linked to good gut health and metabolism. Conversely, sedentary lifestyles can negatively impact the gut causing reduced microbial diversity.
3) Sleep
Poor sleep or lack of sleep can also have harmful effects on microbiome composition. Sleep deprivation can cause a decrease in the diversity of gut microbes, and changes in the abundance of others.
Some studies found that those who suffer from poor sleep had increased levels of harmful gut bacteria Firmicutes and decreases in good bacteria Bacteroidetes. Lack of sleep can also alter the metabolism of gut microbes, which can promote an inflammatory gut lining.
4) Stress
Having high stress levels, especially over long periods of time, can have negative effects on your microbiome composition and how it functions.
Stress can cause shifts in the balance between good and bad gut bacteria. Specifically, we see a decrease in beneficial Lactobacillus and Bifidobacterium and increases in potentially harmful Clostridium and Escherichia coli.
5) Age
Age plays a big role in shaping your microbiome, with diversity and richness changing over time.
Infants have vastly different gut flora composition compared to adults. In early life, the microbiome is much less diverse compared to an adult. However, during this time it changes rapidly.
In adults, the microbiome tends to be stable and well-balanced. As people age and enter their senior years, we start to see shifts again with older adults having reduced microbial diversity and alterations in the number of certain bacterial species.
6) Infections & Disease
There are many infections and diseases that can disrupt the gut microbiome. Some have genetic components, like those discussed above, while others can be related to autoimmune conditions and gastrointestinal infections.
Certain conditions can cause dysbiosis, resulting in an overgrowth of harmful gut bacteria and reducing the number of good bacteria. Some can also disrupt the immune response in the digestive tract, which can cause inflammation and change the composition of microbes that reside there.
Viral infections, such as norovirus, can infect cells that line the gut, and cause changes in the gut microbiome. Some of these effects can be short-term, while others can become chronic, and this can impact your overall health.
7) Medications
Exposure to antibiotics can disrupt the balance of your gut microbiome by disrupting the balance of microorganisms in the digestive tract. These medications can be great for killing off the bad bacteria that can cause infection, but also negatively impact the beneficial bacteria.
Besides antibiotics, other medications such as proton-pump inhibitors and NSAIDs can also affect the gut.
Conclusion
We still have a lot to learn about the genetic impacts on the gut microbiome. What we do know is that there are genetic factors that can impact not only your gut composition but also your gut function. Our understanding of this field continues to expand.
The microbiome is a dynamic ecosystem, affected by genetics, but also diet and lifestyle. Altogether, these things can have downstream effects on many other processes that take place in the body and can positively or negatively impact your health.
While genetics can be useful for understanding your risk for dysbiosis and other gut-related conditions, there is a role for dietary and lifestyle changes to improve microbiome diversity and composition.
Here are some actionable steps you can take today to support the health of your gut microbiome:
- Eat a diverse range of fiber-rich foods and fermented foods
- Limit processed and high-sugar foods
- Avoid unnecessary antibiotic and NSAID use
- Manage stress
- Ensure you get enough sleep
- Exercise regularly
- Stay hydrated
- Consider probiotic supplements
By understanding the role of your microbiome and your genetic risk, you can make informed choices to support your gut health. If you are interested in learning more, consider diving into your own unique genetic profile, and working with a healthcare provider to provide personalized guidance based on your results.
References
- Cahana I, Iraqi FA. Impact of host genetics on gut microbiome: Take‐home lessons from human and mouse studies. Animal Model Exp Med. 2020;3(3):229-236. doi:10.1002/ame2.12134
- Bubier JA, Chesler EJ, Weinstock GM. Host genetic control of gut microbiome composition. Mamm Genome. 2021;32(4):263-281. doi:10.1007/s00335-021-09884-2
- Grieneisen L, Dasari M, Gould TJ, et al. Gut microbiome heritability is nearly universal but environmentally contingent. Science. 2021;373(6551):181-186. doi:10.1126/science.aba5483
- Ley RE, Hamady M, Lozupone C, et al. Evolution of mammals and their gut microbes. Science. 2008;320(5883):1647-1651. doi:10.1126/science.1155725
- The Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402):207-214. doi:10.1038/nature11234
- Hall AB, Tolonen AC, Xavier RJ. Human genetic variation and the gut microbiome in disease. Nat Rev Genet. 2017;18(11):690-699. doi:10.1038/nrg.2017.63
- Lim MY, You HJ, Yoon HS, et al. The effect of heritability and host genetics on the gut microbiota and metabolic syndrome. Gut. 2017;66(6):1031-1038. doi:10.1136/gutjnl-2015-311326
- Goodrich JK, Waters JL, Poole AC, et al. Human genetics shape the gut microbiome. Cell. 2014;159(4):789-799. doi:10.1016/j.cell.2014.09.053
- Goodrich JK, Davenport ER, Beaumont M, et al. Genetic determinants of the gut microbiome in UK twins. Cell Host Microbe. 2016;19(5):731-743. doi:10.1016/j.chom.2016.04.017
- Beaumont M, Goodrich JK, Jackson MA, et al. Heritable components of the human fecal microbiome are associated with visceral fat. Genome Biol. 2016;17(1). doi:10.1186/s13059-016-1052-7
- Million M, Angelakis E, Maraninchi M, et al. Correlation between body mass index and gut concentrations of Lactobacillus reuteri, Bifidobacterium animalis, Methanobrevibacter smithii and Escherichia coli. Int J Obes (Lond). 2013;37(11):1460-1466. doi:10.1038/ijo.2013.20
- Xie H, Guo R, Zhong H, et al. Shotgun metagenomics of 250 adult twins reveals genetic and environmental impacts on the gut microbiome. Cell Syst. 2016;3(6):572-584.e3. doi:10.1016/j.cels.2016.10.004
- Boltin D, Perets TT, Vilkin A, Niv Y. Mucin function in inflammatory bowel disease: An update. J Clin Gastroenterol. 2013;47(2):106-111. doi:10.1097/mcg.0b013e3182688e73
- Smith, A.C. and Podolsky, D. K. Colonic mucin glycoproteins in health and disease. Clinics in Gastroenterology. 1986;15(4):815-837. https://www.ncbi.nlm.nih.gov/pubmed/3536210
- Johansson MEV, Phillipson M, Petersson J, Velcich A, Holm L, Hansson GC. The inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of bacteria. Proc Natl Acad Sci U S A. 2008;105(39):15064-15069. doi:10.1073/pnas.0803124105
- Lehrer RI, Lu W. α-Defensins in human innate immunity: Α-Defensins. Immunol Rev. 2012;245(1):84-112. doi:10.1111/j.1600-065x.2011.01082.x
- Kelly RJ, Rouquier S, Giorgi D, Lennon GG, Lowe JB. Sequence and expression of a candidate for the human secretor blood group α(1,2)fucosyltransferase gene (FUT2). J Biol Chem. 1995;270(9):4640-4649. doi:10.1074/jbc.270.9.4640
- Kashyap PC, Marcobal A, Ursell LK, et al. Genetically dictated change in host mucus carbohydrate landscape exerts a diet-dependent effect on the gut microbiota. Proc Natl Acad Sci U S A. 2013;110(42):17059-17064. doi:10.1073/pnas.1306070110
- Tong M, McHardy I, Ruegger P, et al. Reprograming of gut microbiome energy metabolism by the FUT2 Crohn’s disease risk polymorphism. ISME J. 2014;8(11):2193-2206. doi:10.1038/ismej.2014.64
- Frank DN, St. Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A. 2007;104(34):13780-13785. doi:10.1073/pnas.0706625104
- Tailford LE, Crost EH, Kavanaugh D, Juge N. Mucin glycan foraging in the human gut microbiome. Front Genet. 2015;6. doi:10.3389/fgene.2015.00081
- Bonder MJ, Kurilshikov A, Tigchelaar EF, et al. The effect of host genetics on the gut microbiome. Nat Genet. 2016;48(11):1407-1412. doi:10.1038/ng.3663
- Blekhman R, Goodrich JK, Huang K, et al. Host genetic variation impacts microbiome composition across human body sites. Genome Biol. 2015;16(1). doi:10.1186/s13059-015-0759-1
- Tamburini S, Shen N, Wu HC, Clemente JC. The microbiome in early life: implications for health outcomes. Nat Med. 2016;22(7):713-722. doi:10.1038/nm.4142
- Bennett PR, Brown RG, MacIntyre DA. Vaginal microbiome in preterm rupture of membranes. Obstet Gynecol Clin North Am. 2020;47(4):503-521. doi:10.1016/j.ogc.2020.08.001
- Gupta P, Singh MP, Goyal K. Diversity of vaginal microbiome in pregnancy: Deciphering the obscurity. Front Public Health. 2020;8. doi:10.3389/fpubh.2020.00326
- Ho NT, Li F, Lee-Sarwar KA, et al. Meta-analysis of effects of exclusive breastfeeding on infant gut microbiota across populations. Nat Commun. 2018;9(1). doi:10.1038/s41467-018-06473-x
- Lif Holgerson P, Harnevik L, Hernell O, Tanner ACR, Johansson I. Mode of birth delivery affects oral Microbiota in infants. J Dent Res. 2011;90(10):1183-1188. doi:10.1177/0022034511418973
- Dahl WJ, Rivero Mendoza D, Lambert JM. Diet, nutrients and the microbiome. In: Progress in Molecular Biology and Translational Science. Vol 171. Elsevier; 2020:237-263.
- Zmora N, Suez J, Elinav E. You are what you eat: diet, health and the gut microbiota. Nat Rev Gastroenterol Hepatol. 2019;16(1):35-56. doi:10.1038/s41575-018-0061-2
- Campaniello D, Corbo MR, Sinigaglia M, et al. How diet and physical activity modulate gut Microbiota: Evidence, and perspectives. Nutrients. 2022;14(12):2456. doi:10.3390/nu14122456
- Mohr AE, Jäger R, Carpenter KC, et al. The athletic gut microbiota. J Int Soc Sports Nutr. 2020;17(1). doi:10.1186/s12970-020-00353-w
- Marttinen M, Ala-Jaakkola R, Laitila A, Lehtinen MJ. Gut Microbiota, probiotics and physical performance in athletes and physically active individuals. Nutrients. 2020;12(10):2936. doi:10.3390/nu12102936
- Han M, Yuan S, Zhang J. The interplay between sleep and gut microbiota. Brain Res Bull. 2022;180:131-146. doi:10.1016/j.brainresbull.2021.12.016
- Smith RP, Easson C, Lyle SM, et al. Gut microbiome diversity is associated with sleep physiology in humans. PLoS One. 2019;14(10):e0222394. doi:10.1371/journal.pone.0222394
- Madison A, Kiecolt-Glaser JK. Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr Opin Behav Sci. 2019;28:105-110. doi:10.1016/j.cobeha.2019.01.011
- Badal VD, Vaccariello ED, Murray ER, et al. The gut microbiome, aging, and longevity: A systematic review. Nutrients. 2020;12(12):3759. doi:10.3390/nu12123759
- Conway J, A Duggal N. Ageing of the gut microbiome: Potential influences on immune senescence and inflammageing. Ageing Res Rev. 2021;68(101323):101323. doi:10.1016/j.arr.2021.101323
- González R, Elena SF. The interplay between the host microbiome and pathogenic viral infections. MBio. 2021;12(6). doi:10.1128/mbio.02496-21
- Trakman GL, Fehily S, Basnayake C, et al. Diet and gut microbiome in gastrointestinal disease. J Gastroenterol Hepatol. 2022;37(2):237-245. doi:10.1111/jgh.15728
- Weersma RK, Zhernakova A, Fu J. Interaction between drugs and the gut microbiome. Gut. 2020;69(8):1510-1519. doi:10.1136/gutjnl-2019-320204