
Nutrigenomics and How to Personalize Your Nutrition


Nutrigenomics and How to Personalize Your Nutrition
What is nutrigenomics?
Nutrigenomics is the field of study that examines the impact of nutrition and genes on health. Your genes determine your tendency to respond to or process certain nutrients, either in the short or long-term.
By “nutrients”, we are largely referring to macronutrients (carbohydrates, fat, protein) and micronutrients (vitamins and minerals). Genetic variations can impact the way your body digests and utilizes these nutrients. Conversely, nutrients can affect the function of genes and the bodily processes they regulate.

Genetic testing technologies can reveal what genetic variants you have. Understanding how these variants affect each gene function is a needle in a haystack problem (aka very difficult) as everyone has 4 – 5 million single nucleotide variants. Scientists use gene association studies, which analyze population traits with variant data to understand how each variant is associated with a trait. By working with a practitioner who can help you pinpoint the right variants to work on, you can make personalized decisions regarding diet and supplementation.
For example, if your body’s detox pathways are suboptimal, you can use nutrients and building blocks to support those genes and detox pathways. If your body doesn’t make adequate amounts of an active form of a nutrient due to your genetic makeup, this can have negative health consequences. In this case, you can supplement with the active form to improve your health.
With the number of genes involved in nutrient-related functions, the possibilities for using nutrigenomics to optimize your health are vast.
How does nutrigenomic testing work?
There are direct-to-consumer (DTC) genetic tests that you can purchase yourself, and FDA-regulated clinical genetic tests that require a medical prescription. While they may use the same technologies, for the purpose of this article, let’s focus on DTC tests.
The first step involves purchasing a test kit shipped to your home and sending in your samples. Since every cell in your body contains the same DNA, the sample collection is simple. Some companies collect saliva, while others collect blood or a swab of the side of your cheeks.
You then cap the tube and mail it to the lab. They will then determine your genetic variants and provide you with the results in 2 – 6 weeks.
Currently, three different types of direct-to-consumer genetic tests are available, based on the type of variants they test for.
- Single nucleotide polymorphism (SNP, or pronounced Snips)
- Whole genome sequencing
- Exome testing
Importantly, none of these tests for your nutrient levels. Rather, these data may indicate your tendency to respond to process certain nutrients.
SNP Testing
SNP is the most common genetic test, provided by companies such as 23andMe and Ancestry.
Your genetic codes in your DNA are basically a series of letters. Imagine a gene has a typical letter code of AATTCC. Each letter is called a nucleotide. If one of these nucleotides in your gene is different from the typical one (a polymorphism), then you have a single nucleotide polymorphism, or a SNP. To provide an example using the gene code of AATTCC, you could find out from your nutrigenomic SNP report that your gene has a code of AATACC. This gene has a SNP in the second “T” in the code.
Most SNPs don’t affect gene function at all, but a small percentage of them either increase or decrease gene function. The latter may affect your health risks.
Whole genome sequencing
This technology gives you almost all the DNA sequences in your entire genome. Therefore, it gives a lot more information than SNP testing, such as:
- Deletion of a segment of your DNA (insertion)
- Addition of a segment of your DNA (deletion)
- Increased copy numbers of certain genes (copy number variations)
The downside of whole-genome sequencing is that it’s quite expensive ($399 to over $1000 currently), especially if only 2% of the human genomes are genes. So, you’re paying to sequence a lot of fluff DNA, although sometimes there is important DNA outside of the 2%. The cost is going down as the technology improves, though.
Exome sequencing
Exome sequencing focuses on sequencing only the active parts of your genes, which eliminates the main downside of whole-genome sequencing.
Each protein-coding gene has two primary types of sequences called introns and exons. Exons are the part of the gene that gets read into proteins. They’re the “active” part of the gene. Introns do not code for proteins but serve other functions. An exome is all the exons you have in your entire genome. So, while whole genome sequencing gives you everything (introns, exons, and more), exome testing just gives you the exons.
This is a nice feature because after all, what you’re interested in is the code of the exons that gets read into proteins. The intron is often (not always) unneeded information, after all. Other than this point, exome testing carries the same pros, cons, and considerations as whole genome testing.
For each of these tests, you’ll receive a report that tells you your variants. Some companies will also flag the variants by genes that matter the most. Some will also provide remedies or recommendations based on the genes.
How should you approach nutrigenomics?
Your genome is vast, so these reports give a lot of data! Interpreting them and knowing which genes to focus on is complex. It’s critically important that you don’t focus on one gene or think you’re doomed because of it.
The best thing to do is work with a practitioner who knows how to work with these data. They’ll look at your genes through the lens of epigenetics, your clinical history, and your health concerns. They can then explain to you what your variants mean and how you can best optimize your health based on the data.
There are many types of practitioners who can help, such as
- Naturopathic and functional medicine doctors
- Nutrigenomic/genetic counselors
- Nutritionist or dieticians
You want to make sure that they’re trained to use nutrigenomic data and routinely use them with their patients.
Keep in mind, though, that nutrigenomic testing is not for everyone. For example it can reveal a disease risk you may not want to know about yourself or your relatives. Cases also have been reported when people find out they’re not related to their family member they thought are related. Lastly, there are also privacy concerns as some nutrigenomic companies profit from selling their customer data. You should do your own research and understand these risks before sending in your samples.
Hierarchy of genes to address in nutrigenomics
For the best chance of succeeding with nutrigenomics, it is best to follow a system where foundational components of health are addressed in an ascending order.
A common mistake a lot of newbies make is jumping straight to fixing methylation, which can often lead to bad reactions that can set people back in their health journey.
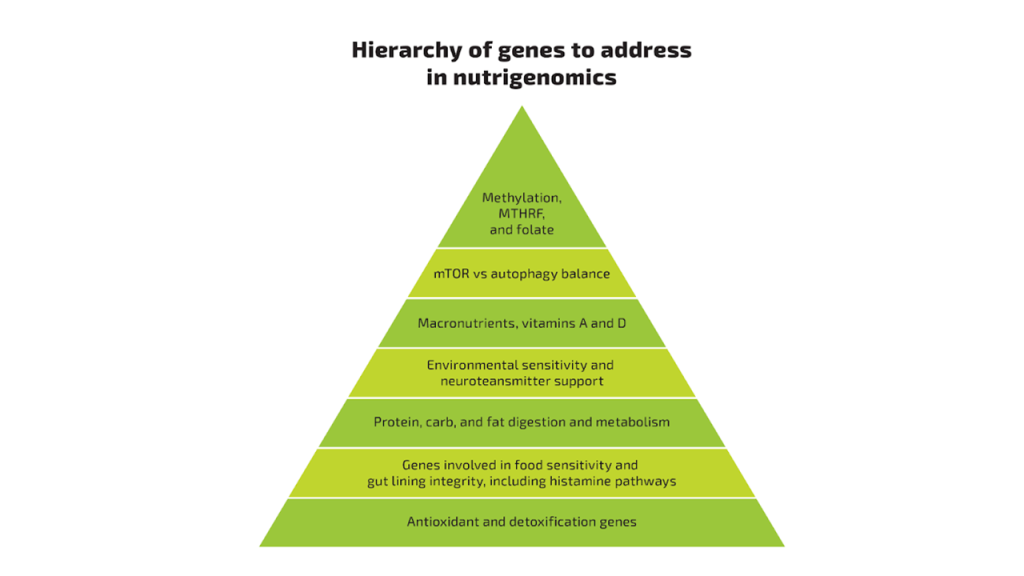
BIOptimizers has developed this nutrigenomic pyramid that can help you address each piece in a logical order, where each component builds on the next. You want to start from the bottom, optimize that area, then move on to the next layer.The same goes for optimizing other areas before the ones below.
Below is a description of each level of the pyramid, starting at the bottom.
Antioxidant and detoxification genes
These are at the bottom because when your body can’t detoxify or maintain a balance of oxidative stress, it tends to throw off most other bodily functions. The more of an imbalance there is in these areas, the worse symptoms you will experience.
A common effect of “pushing” your body to work harder in higher levels of the pyramid is that there is more “junk” for your body to detoxify. This isn’t a problem if your detox pathways work well. However, if they don’t and you start burdening your detoxification system heavily, the system gets backed up and your body starts to get overloaded.
This overload causes a situation where you feel crummy because your body can’t detox appropriately, leading to more inflammation and oxidative stress. If this is the case, you will likely not feel better until you get these systems working well.
Genes involved in food sensitivity, gut lining integrity, including histamine pathways
The gut is a primary barrier between the outside world and inside your body. Things you eat aren’t technically inside your body until they’re absorbed. Your gut is highly specialized to maintain a tight barrier so that only appropriate things get across. When this barrier is weak, it is often termed “leaky gut”. Leaky gut leads to immune system overactivation, inflammation, and increases the risk for a number of health conditions, including autoimmunity.
Food sensitivities can contribute to inflammation in the gut and your whole body. One way is through activating the immune system in your gut and potentially contributing to leaky gut.
Histamine is both an inflammatory mediator and neurotransmitter. Too much histamine or a genetic weakness in the ability to break down histamine can lead to issues in the digestive system, cardiovascular system, and can strongly influence mood and emotions.
Due to the importance of the gut lining, and the commonality of histamine and food sensitivities contributing to symptoms, you want to work on genes in this category second.
Protein, carb, and fat digestion and metabolism genes
Protein, carbohydrates, and fats are termed “macronutrients”. Your body needs these in large amounts for healthy functioning. Proteins provide building blocks for your body and are necessary for everything from building every enzyme in your body, to synthesizing neurotransmitters. Carbohydrates are a primary energy form for every cell in your body. Fat is also an energy form for cells that also plays essential roles in cell signaling, hormone synthesis, and promoting a healthy inflammatory response.
You want to address the genes in this category through diet and supplementation. For example, some people genetically do better with keto, while others do better with carbs. Genes can also influence your ability to digest these foods, so you want to supplement accordingly.
Environmental sensitivity and neurotransmitter genes
No matter how “clean” we live, the reality is that we are all exposed regularly to environmental toxins. Any genes that affect how you are impacted from things like chemicals in the environment is important to address sooner than later. The ability to deal with and detox environmental toxins has a profound effect on overall health. They can cause inflammation, oxidative stress, interfere with hormonal function, and disrupt normal cellular metabolism.
Neurotransmitters are the language of the nervous system. It’s how your brain communicates between different regions and also how your nervous system communicates in the rest of your body. In your brain, problems with neurotransmitter balance can contribute to poor memory, cognitive problems, brain fog, and altered mood. Other places in your body can be impacted in areas like the digestive and cardiovascular system.

Vitamins A and D genes
Among the many roles of these two nutrients, one of the most important is their necessity for healthy immune system function. Immune system dysfunction and imbalance underlies many chronic health problems. Vitamin A and D also help the gut lining remain strong and the gut immune system stay healthy.
For each of these vitamins, your body requires them to be in an active form. If you have any genetic variants that reduce your ability to activate or receive signals from these vitamins, you’ll need to be sure you get enough of the right forms to prevent deficiencies.
mTOR versus autophagy balance genes
mTOR (mammalian target of rapamycin) is your cellular nutrient sensor. In response to nutrients and energy supply, mTOR promotes cells to grow when there is plenty of energy, and die and recycle when there is an absence of nutrition, such as with fasting.
To maintain healthy cells, you cycle between fasting and eating modes. During fasting, low mTOR function, apoptosis (death of unhealthy cells), and autophagy (the separating and reuse of old cell parts) happen. The mTOR protein regulates these vital balances between growth and cleaning up.
If these processes are impaired, the body cannot “clean up” appropriately. Altered mTOR activity can contribute to unstable DNA and is associated with several different types of cancers.
Methylation, MTHFR, and Folate
MTHFR and methylation (or one-carbon metabolism) have been the most-studied and thus most popular genes in nutrigenomic. Many with chronic and unexplained symptoms want to look into MTHFR for a possible answer to their health issues.
MTHFR is the bottleneck gene that helps activate folate into methylfolate. You then need the methylfolate to feed the methylation cycle. Methylation is a basic chemical reaction in your body that regulates numerous cellular processes. If your body doesn’t methylate well, it can cause problems in many bodily systems such as the cardiovascular and nervous systems, as well as your ability to detoxify appropriately.
While it is clearly important to address a problem with MTHFR and methylation, jumping straight to taking high doses of activated folate and “pushing” the methylation cycle can cause a lot of side effects and distressing symptoms if you don’t address the lower tiers of the nutrigenomic hierarchy first.

Examples of how understanding your genes can improve your nutrition
Vitamin A plays important roles in vision, embryonic development, cell differentiation, healthy mucus membranes and skin, as well as immune function. In order for vitamin A to work, it has to be activated by the enzyme BCO1 (beta-carotene oxygenase 1). It also goes by these acronyms: BCO; BCDO; BCMO; BCDO1; BCMO1.
If there is a genetic variant of BCO1 that reduces the enzyme function, your body can have a difficult time converting beta-carotene from plants to the active form of vitamin A, called retinol. Many animal products naturally contain retinol. An implication of this is that someone with a BCO1 gene mutation, needs to eat animal products. They may not do well long term with a plant-based diet due to this poor conversion, unless they supplement with retinol.
Similarly, your body needs essential fatty acids. Two of these are the omega-3 fatty acids DHA and EPA, found in cold water fish oil. Many plants contain omega-3’s in the form of alpha-linolenic acid (ALA). Humans can convert ALA into EPA and DHA, but it is quite inefficient, especially with genetic variants that further reduce this conversion. If you have a variant that weakens your delta-6-desaturase gene, you’ll need to make sure that you’re getting EPA and DHA from food or supplements.
Conclusion
Nutrigenomics is a relatively new and rapidly expanding field, offering you the most precise and personalized diet and nutrition information available. If you want to unlock the next level of health optimization, or you have symptoms that aren’t improving with other approaches, nutrigenomics may provide the missing pieces to the puzzle.
BIOptimizers will soon be releasing our own book on personalized nutrition to help guide you towards more optimal health. If you want to know when this becomes available, sign up for the waiting list and we’ll be in touch as soon as the book is out!
References
- Zou Z, Tao T, Li H, Zhu X. mTOR signaling pathway and mTOR inhibitors in cancer: progress and challenges. Cell Biosci. 2020;10(1):31. doi:10.1186/s13578-020-00396-1
- Zining J, Lu X, Caiyun H, Yuan Y. Genetic polymorphisms ofmTORand cancer risk: a systematic review and updated meta-analysis. Oncotarget. 2016;7(35):57464-57480. doi:10.18632/oncotarget.10805
- Vidmar Golja M, Šmid A, Karas Kuželički N, Trontelj J, Geršak K, Mlinarič-Raščan I. Folate insufficiency due to MTHFR deficiency is bypassed by 5-methyltetrahydrofolate. J Clin Med. 2020;9(9):2836. doi:10.3390/jcm9092836
- BCO1 beta-carotene oxygenase 1 [Homo sapiens (human)] – Gene – NCBI. Nih.gov. Accessed November 29, 2022. https://www.ncbi.nlm.nih.gov/gene/53630
