5 Ways To Optimize Your Immune System For Back To School


5 Ways To Optimize Your Immune System For Back To School
One of the few things kids don’t mind sharing is germs. They go to school, pick up germs, and bring them home. On top of that, as the weather turns colder, we spend more time in close contact with others indoors, making it harder to avoid exposure to others who are sick.
As a result, many parents are constantly sick.
If your immune system is strong, you don’t have much to worry about. However, many people have immune systems that don’t function at their full potential. Luckily, there are things you can do to support healthy immune function
Immune System Basics
Before I get into the good stuff, I want to teach you some immune system basics. Your defense system comprises two parts:
- The innate immune system, which responds immediately
- Your adaptive immune system, which learns and applies information to future infections. This allows your body to clear out remembered infections faster and more effectively.

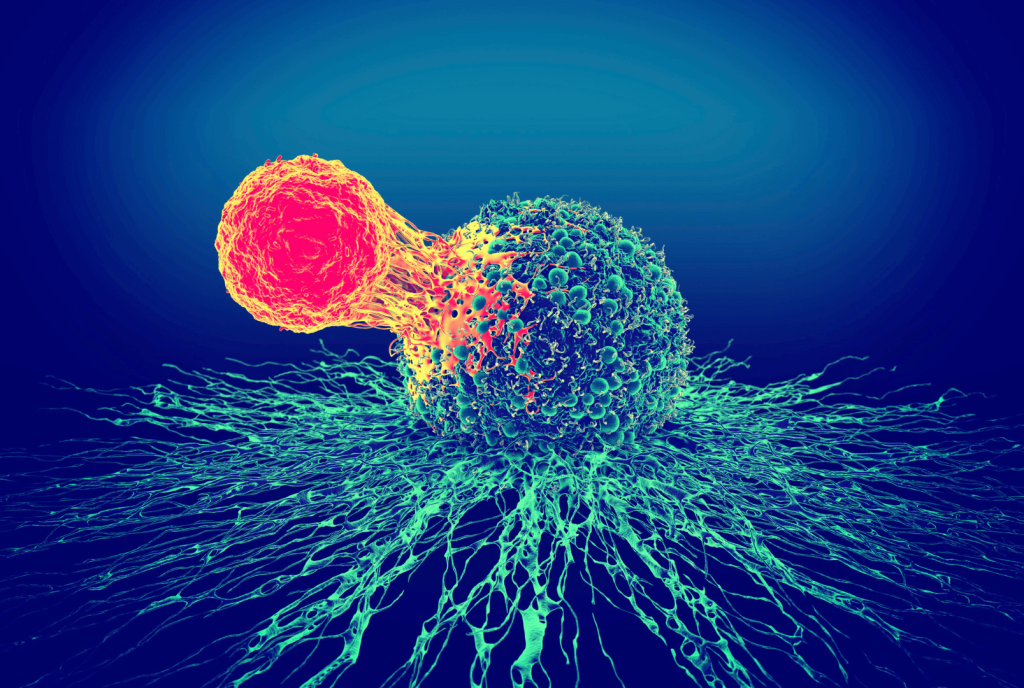
The innate immune system can identify the difference between self and others and immediately responds when it detects something that doesn’t belong inside your body. The response triggers the arrival and attack by cells called neutrophils, followed by macrophages that attack bacteria and viruses.
When macrophages encounter an enemy, they release cytokines, which are small proteins that carry information. The presence of cytokines kicks your immune cells into action and tells the immune cells where to go and fight.
Cytokines also carry the information that kicks the adaptive immune system into gear. Your adaptive immune system pulls from its large library of information to deploy the most appropriate forces to defend your body.
Once the adaptive immune system knows what it’s dealing with, it responds with lymphocytes (a kind of white blood cell) in two different ways. First, it sends specialized T cells to target the specific intruder. Second, it activates B cells to begin pumping out antibodies.
If part of your immune system is not working optimally, you’re more likely to get sick. Now, there are two aspects of immune system optimization: readiness and balance. For example, a hyperactive immune system can be off-balance and attack things it shouldn’t, such as allergens and your own cells.
Continue reading to learn ways you can give your immune system what it needs to ensure it’s in proper fighting form.
1. Optimize Your Sleep
Sleep is crucial for both immune readiness and balance. Many of us know that sleep deprivation makes you more likely to get sick. Those with allergies or autoimmune disease also know that poor sleep can make it worse or cause flares.
While you’re sleeping, your body is busy at work making cytokines to produce an immune response and T cells to fight infection. When you don’t get enough sleep, your body cannot produce as many T cells, leaving your body without as much immune protection. A decrease in cytokines due to sleep deprivation can lead to a weaker immune system.
Not getting enough sleep increases your risk of getting a cold. In a study of 164 healthy adults, scientists monitored participants’ sleep for seven days before exposing participants to the common cold via nasal drops. For five days after exposure, scientists swabbed participants’ noses for infection. Those who slept between 5 and 6 hours a night were at greater risk than those who got more than 6 hours of sleep. Therefore, more sleep can reduce your risk of catching a cold.
Sleep also plays a crucial role in your adaptive immune system’s ability to remember previous infections and know how to attack. A meta-study examined vaccine studies and the impact of sleep deprivation on the immune response. Participants maintaining a normal sleep schedule versus sleep-deprived showed double the number of antibodies.
You are automatically putting your body at a higher risk of getting sick without enough sleep or with low-quality sleep. Check our sleep optimization post for some great tips if you struggle to get enough sleep.
2. Ensure Vitamin D And Magnesium Are At Healthy Levels
Vitamin D
Vitamin D is widely known to support a healthy immune system. It’s a key signaling molecule in both your innate and adaptive immune systems.
In the innate immune system, your body’s first line of defense, vitamin D regulates the production and activity of antiviral attackers like neutrophils and macrophages. It stimulates these cells to produce antimicrobial peptides in the lining of your lungs, noses, and respiratory tracts. These peptides act as antivirals and can deactivate the viruses before they can bind to your cell surface. That means people with healthy vitamin D levels are less likely to catch sniffles.
Vitamin D goes to work in your adaptive immune system by regulating the production of T cells. Remember that your T cells release cytokines. Cytokines can either be inflammatory or anti-inflammatory. When bacteria or a virus invades your body, vitamin D tells your body to produce more anti-inflammatory cytokines and decrease the production of proinflammatory cytokines. This is why a vitamin D deficiency is associated with complications from colds and flus, including pneumonia.
When your vitamin D levels are low, both your immune readiness and balance will be suboptimal. Adults with low vitamin D levels are more likely to experience upper respiratory infections. A study of 18,883 individuals ages 12+ analyzed the relationship between vitamin D levels and the rate of upper respiratory infection. Participants who experienced a recent upper respiratory infection also had lower levels of vitamin D than those without.
This brings us to the question, what are optimal vitamin D levels? In the study mentioned above, participants with vitamin D levels of 30 ng/mL or higher had the lowest incidence of infection. Other studies identify a range of 25 – 80 ng/mL based on the levels found in healthy individuals. Either way, dipping below 25 ng/mL isn’t optimal. A blood test can tell you what your current vitamin D levels are.
When supplementing with vitamin D, how much should you take? While following recommended dietary allowances (RDAs) seems like a safe bet, it’s not. You are very unlikely to reach the optimal vitamin D levels of 25 ng/mL by consuming the recommended maximum of 600 IU/d per day.
A meta-analysis of 108 studies examined the optimal vitamin D supplementation amount needed to achieve vitamin D levels of 25 ng/mL. 97.5% of healthy individuals needed around 3,000 IU of vitamin D daily. Obese individuals needed around 7,000 IU per day. Therefore, you should take at least 3,000 IU of vitamin D daily.
Everyone is different, so the best thing to do is to get a blood test with your doctor seasonally, especially if you live in colder climates. Then, figure out the dose that keeps your blood vitamin D levels in the healthy range.
Magnesium
Magnesium is also critical for immune system function and an essential cofactor to help activate Vitamin D. When your magnesium levels are low, your T cells can’t do their job of seeking out and destroying invaders.
Remember that immune cells release cytokines to provide information to tell your adaptive immune system exactly how to respond. Low magnesium levels decrease your cytokines production. Fewer cytokines means less information for an appropriate response. Additionally, when magnesium is deficient, you are more likely to produce proinflammatory cytokines rather than anti-inflammatory ones.
At least 50% of the population fail to get 50% of the recommended daily allowance, or the bare minimum intake of magnesium each day. This means magnesium deficiencies are extremely common.
Magnesium deficiencies can make the airway more reactive and spasmic to irritants. At the same time, since magnesium is essential for over 300 biochemical reactions in your body, a magnesium deficiency can weaken immune functions. Magnesium is also important to help your airway muscles relax and immune cells stay balanced.
Vitamin D and magnesium are independently important for the immune system. Together, they are even more beneficial since magnesium activates vitamin D.
Knowing what kind of magnesium to take can be confusing. Magnesium Breakthrough has all seven types of magnesium to support multiple critical body functions, including activating vitamin D and supporting healthy immune functions.
3. Use Medicinal Mushrooms And Probiotics
Medicinal Mushrooms
Medicinal mushrooms have a long-established history of use in traditional medicine. Mushrooms like Reishi, Shiitake, and Chaga have been in use for hundreds, possibly thousands, of years in Eastern medicine.
Medicinal mushroom extracts can stimulate the production of certain cytokines from immune cells, such as lymphocytes and macrophages. They can also stimulate your B cells to produce healthy levels of antibodies.
These mushrooms support your immune readiness while also supporting immune balance. It doesn’t tend to worsen allergies or autoimmunity. These properties make medicinal mushrooms a great way to support immune readiness and gut health.

Some of the superstars of medicinal mushrooms are:
- Reishi (Ganoderma lucidum) stimulates your immune cells and helps modulate your immune response.
- Chaga (Inonotus obliquus) support natural immune defenses.
- Shiitake (Lentinus edodes) improves immune function by increasing immune cell production and antibodies and balancing inflammation.
- Turkey Tail (trametes versicolor) is an antioxidant, anti-inflammatory, and promotes healthy gut flora, supporting natural immune defense against viruses and bacteria.
- Cordyceps (Cordyceps sinensis) supports innate and adaptive immune systems and regulates gut flora.
- Lion’s Mane (Hericium Erinaceus) supports healthy immune cell activity throughout your body and, more specifically, in your gut by supporting your mucosal lining.
You can find many of these medical mushrooms and more in Mushroom Breakthrough to support your immune system and boost your brain power.
Probiotics
Somewhere between 70-80% of your immune cells are in your gut. Your gut is filled with good, neutral, and bad bacteria living on top of the protective mucosal barrier. This barrier includes the protective mucus and a layer of epithelial cells. If your gut bacteria get on the other side of this barrier, they’re one step closer to getting into your bloodstream and causing trouble.
Your immune system constantly monitors this area to make sure nothing is trying to get through.
The final layer of defense in your gut is where most of your immune system is. It’s filled with macrophages waiting to attack and B cells ready to produce antibodies.
Probiotics, the good bacteria in your gut, are the key to keeping your gut, and therefore most of your immune system, healthy. Probiotics increase the number of bacteria-killing macrophages in the gut and promote the survival of your epithelial cells. One of the most important roles of probiotics is keeping the immune system balanced by enhancing your innate immune system and decreasing inflammation.
A meta-analysis of 33 clinical studies examined probiotics’ effectiveness on respiratory infections. 28 studies reported some benefits. The other 5 showed no obvious benefit. Therefore, probiotics may support your body’s immune readiness.
Probiotics also play a critical role in preventing and healing leaky gut. Leaky gut occurs when the protective layers of your gut are damaged and undigested food, toxins, and bacteria penetrate through it. Your gut can’t work optimally as your immune system if you have a leaky gut.
Leaky gut also prevents you from enjoying the immune-boosting benefits of Vitamin D. Vitamin D depends on the body’s ability to absorb it through the gut. A leaky gut can prevent you from absorbing what you need to support a healthy immune system.
Biome Breakthrough doesn’t only heal your gut with its probiotic and prebiotic blend, but also nourishes your gut lining with collagen and bone broth. The IgYmax in Biome Breakthrough can safely and specifically bind bad gut bacteria and help expel them to make room for a better gut flora.
4. Use Immune Nutrients
If you start to feel a cold or flu coming on, grab some zinc and vitamin C for immune system support.
Zinc
Zinc is a critical mineral for the development and function of both your innate and adaptive immune cells. It reduces oxidative stress and inflammation. Zinc deficiency leads to impaired immune response. The good news is that adequate zinc supplementation can easily replenish your zinc levels and reverse these effects.
Zinc can reduce the severity and duration of a cold, but you have to start taking it early. A meta-analysis examined the use of zinc to treat the common cold. Patients took between 10 and 24 mg of zinc daily within 24 hours of experiencing cold symptoms. Compared to a placebo group, patients who took zinc had shorter colds.
Zinc can also prevent you from getting sick. The same meta-analysis examined studies that administered zinc to children ages 6.5 to 10 years old preventatively. 394 children received between 10-15mg of zinc daily for 5 to 7 months or a placebo. Those who received zinc had fewer colds.
Start taking zinc now to help prevent coming down with a cold or at the very least within 24 hours of experiencing symptoms. All-around, correcting a zinc deficiency allows your immune system to work at its full potential.

Vitamin C
Vitamin C is an essential nutrient. It supports your body as an antioxidant and by strengthening your epithelial barrier in your gut. Vitamin C lends additional support to your immune system by stimulating the activity of your T cells and B cells. All around, it’s an immune super supporter.
Taking vitamin C can shorten your cold. A meta-analysis of 31 studies examined the effects of vitamin C on the common cold. In both adults and children, vitamin C shortened the duration of the cold and reduced its severity.
Your body can’t make vitamin C on its own. Stress, infections, travel, illness, and wound healing all increase your need for vitamin C. The best way to get high amounts of vitamin C is through supplements. 1,000 to 2,000 mg per day is an effective and safe dosage to shorten your cold and support your immune system.
5. Manage Stress
Chronic stress is one of your body’s worst enemies when it comes to maintaining a strong immune system. When you’re stressed, your body’s ability to shut down inflammation is impaired leading to chronic inflammation. Stress can also cause your T cells to make the wrong decision about how to respond. When you’re stressed, your body releases cortisol, which suppresses your immune system.
A meta-analysis examined studies covering 30 years of research on the relationship between stress and the immune system. With 18,941 total participants, researchers determined that brief short-term stress, such as public speaking, actually improves the immune system. The number of immune cells increases as your body gets prepared to fight or flight and to heal any potential wounds.
When the stress becomes chronic, however, it significantly weakens your immune function. The same meta-analysis showed that participants experiencing chronic stress had decreased function of both their innate and adaptive immune systems.
Managing stress and taking time out for yourself regularly can keep you going strong throughout the cold and flu season. Some methods backed by science include:
- Yoga
- Mindfulness
- Enjoying some music
- Regular exercise
- Visiting nature
- Having a cup of tea
For more tips on how to combat stress, check out this blog post.
The Takeaway
You might not be able to avoid germ exposure, but you can take steps to strengthen your immune system. A strong immune system can help you fight germ exposure and bounce back faster if you get sick. Start taking protective measures now to prevent sickness during cold and flu season.
References
- Dettmer P. Immune: A Journey into the Mysterious System That Keeps You Alive. Random House; 2021.
- Alberts B, Johnson A, Lewis J, Raff M, Roberts K, Walter P. The Adaptive Immune System. Garland Science; 2002.
- Bollinger T, Bollinger A, Skrum L, Dimitrov S, Lange T, Solbach W. Sleep-dependent activity of T cells and regulatory T cells. Clin Exp Immunol. 2009;155(2):231-238. doi:10.1111/j.1365-2249.2008.03822.x
- Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally assessed sleep and susceptibility to the common cold. Sleep. 2015;38(9):1353-1359. doi:10.5665/sleep.4968
- Besedovsky L, Lange T, Haack M. The sleep-immune crosstalk in health and disease. Physiol Rev. 2019;99(3):1325-1380. doi:10.1152/physrev.00010.2018
- Bryson KJ, Nash AA, Norval M. Does vitamin D protect against respiratory viral infections? Epidemiol Infect. 2014;142(9):1789-1801. doi:10.1017/S0950268814000193
- Barlow PG, Svoboda P, Mackellar A, et al. Antiviral activity and increased host defense against influenza infection elicited by the human cathelicidin LL-37. PLoS One. 2011;6(10):e25333. doi:10.1371/journal.pone.0025333
- Martineau AR, Jolliffe DA, Greenberg L, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol Assess. 2019;23(2):1-44. doi:10.3310/hta23020
- Bui L, Zhu Z, Hawkins S, Cortez-Resendiz A, Bellon A. Vitamin D regulation of the immune system and its implications for COVID-19: A mini review. SAGE Open Med. 2021;9:20503121211014070. doi:10.1177/20503121211014073
- Zhou YF, Luo BA, Qin LL. The association between vitamin D deficiency and community-acquired pneumonia: A meta-analysis of observational studies: A meta-analysis of observational studies. Medicine (Baltimore). 2019;98(38):e17252. doi:10.1097/MD.0000000000017252
- Ginde AA, Mansbach JM, Camargo CA. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the third national health and nutrition examination survey. Arch Intern Med. 2009;169(4):384. doi:10.1001/archinternmed.2008.560
- Kennel KA, Drake MT, Hurley DL. Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc. 2010;85(8):752-757; quiz 757-758. doi:10.4065/mcp.2010.0138
- Institute of Medicine, Food and Nutrition Board, Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. National Academies Press; 1999.
- Veugelers PJ, Pham TM, Ekwaru JP. Optimal vitamin D supplementation doses that minimize the risk for both low and high serum 25-hydroxyvitamin D concentrations in the general population. Nutrients. 2015;7(12):10189-10208. doi:10.3390/nu7125527
- University of Basel. Magnesium is essential for the immune system, including in the fight against cancer. Science Daily. Published online January 19, 2022. Accessed October 15, 2022.
- DiNicolantonio JJ, O’Keefe JH. Magnesium and vitamin D deficiency as a potential cause of immune dysfunction, cytokine storm and disseminated intravascular coagulation in covid-19 patients. Mo Med. 2021;118(1):68-73.
- Lull C, Wichers HJ, Savelkoul HFJ. Antiinflammatory and immunomodulating properties of fungal metabolites. Mediators Inflamm. 2005;2005(2):63-80. doi:10.1155/MI.2005.63
- Teplyakova TV, Ilyicheva TN, Kosogova TA, Wasser SP. Medicinal mushrooms against influenza viruses. Int J Med Mushrooms. 2021;23(2):1-11. doi:10.1615/IntJMedMushrooms.2020037460
- Zhang J, Tang Q, Zimmerman-Kordmann M, Reutter W, Fan H. Activation of B lymphocytes by GLIS, a bioactive proteoglycan from Ganoderma lucidum. Life Sci. 2002;71(6):623-638. doi:10.1016/s0024-3205(02)01690-9
- Kim YR. Immunomodulatory activity of the water extract from medicinal mushroom Inonotus obliquus. Mycobiology. 2005;33(3):158-162. doi:10.4489/MYCO.2005.33.3.158
- Dai X, Stanilka JM, Rowe CA, et al. Consuming Lentinula edodes (shiitake) mushrooms daily improves human immunity: A randomized dietary intervention in healthy young adults. J Am Coll Nutr. 2015;34(6):478-487. doi:10.1080/07315724.2014.950391
- Yu ZT, Liu B, Mukherjee P, Newburg DS. Trametes versicolor extract modifies human fecal microbiota composition in vitro. Plant Foods Hum Nutr. 2013;68(2):107-112. doi:10.1007/s11130-013-0342-4
- Lin BQ, Li SP. Cordyceps as an Herbal Drug. In: Oxidative Stress and Disease. CRC Press; 2011:73-105.
- Sheng X, Yan J, Meng Y, et al. Immunomodulatory effects of Hericium erinaceus derived polysaccharides are mediated by intestinal immunology. Food Funct. 2017;8(3):1020-1027. doi:10.1039/c7fo00071e
- Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. The interplay between the gut microbiome and the immune system in the context of infectious diseases throughout life and the role of nutrition in optimizing treatment strategies. Nutrients. 2021;13(3):886. doi:10.3390/nu13030886
- Yan F, Polk DB. Probiotics and immune health. Curr Opin Gastroenterol. 2011;27(6):496-501. doi:10.1097/MOG.0b013e32834baa4d
- Lehtoranta L, Pitkäranta A, Korpela R. Probiotics in respiratory virus infections. Eur J Clin Microbiol Infect Dis. 2014;33(8):1289-1302. doi:10.1007/s10096-014-2086-y
- Wessels I, Maywald M, Rink L. Zinc as a gatekeeper of immune function. Nutrients. 2017;9(12). doi:10.3390/nu9121286
- Ibs KH, Rink L. Zinc-altered immune function. J Nutr. 2003;133(5):1452S-1456S. doi:10.1093/jn/133.5.1452s
- Rao G, Rowland K. PURLs: Zinc for the common cold–not if, but when. J Fam Pract. 2011;60(11):669-671.
- Carr A, Maggini S. Vitamin C and immune function. Nutrients. 2017;9(11):1211. doi:10.3390/nu9111211
- Hemilä H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. 2013;2013(1):CD000980. doi:10.1002/14651858.CD000980.pub4
- Bucher A, White N. Vitamin C in the prevention and treatment of the common cold. Am J Lifestyle Med. 2016;10(3):181-183. doi:10.1177/1559827616629092
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130(4):601-630. doi:10.1037/0033-2909.130.4.601
- Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4(2):49-54. doi:10.4103/0973-6131.85485
- Sharma M, Rush SE. Mindfulness-based stress reduction as a stress management intervention for healthy individuals: a systematic review: A systematic review. J Evid Based Complementary Altern Med. 2014;19(4):271-286. doi:10.1177/2156587214543143
- de Witte M, Spruit A, van Hooren S, Moonen X, Stams GJ. Effects of music interventions on stress-related outcomes: a systematic review and two meta-analyses. Health Psychol Rev. 2020;14(2):294-324. doi:10.1080/17437199.2019.1627897
- Elliott LD, Wilson OWA, Holland KE, Bopp M. Using exercise as a stress management technique during the COVID-19 pandemic: The differences between men and women in college. Int J Exerc Sci. 2021;14(5):1234-1246.
- Ewert A, Chang Y. Levels of nature and stress response. Behav Sci (Basel). 2018;8(5). doi:10.3390/bs8050049
- Steptoe A, Gibson EL, Vuononvirta R, et al. The effects of tea on psychophysiological stress responsivity and post-stress recovery: a randomised double-blind trial. Psychopharmacology (Berl). 2007;190(1):81-89. doi:10.1007/s00213-006-0573-2
