How To Maintain Stable Blood Sugar Levels
How To Maintain Stable Blood Sugar Levels
What is unstable blood sugar, and what causes it?

Glucose is an important energy source for all cells, especially your brain, so you want a steady supply of glucose in your blood. However, glucose is also an oxidizing sugar, so having too high a glucose level can cause oxidative damage to your blood vessels and tissues.
Typically, unstable blood sugar starts with high blood sugar from eating a high-carbohydrate or sugary meal, which triggers a surge of insulin. Subsequently, the insulin quickly puts the glucose into your fat and muscle cells, causing the blood sugar to drop quickly.
The drop in blood sugar triggers stress hormones like adrenaline and cortisol, which may cause mental distress and irritability. Also, you start to feel ravenous hunger and crave more sugary foods to increase your blood sugar. The cycle continues in a blood sugar rollercoaster.
Many people oscillate between high and low blood sugar until, eventually, their cells stop being able to respond to insulin as healthy cells should . So, both your baseline and post-meal blood sugar become higher. As this happens, you may notice a growing midsection, as fat cells in this region collect blood sugar even when other cells stop responding to insulin.
If you don’t fix unstable blood sugar, the pancreas can start to burn out from producing so much insulin, and this can lead to type II diabetes in 10 to 15 years .
Other than high-carb or sugary meals, other causes of unstable blood sugar may include:
- Lack of physical activity
- Stress
- Side effects from medications
- Hormonal changes (due to unhealthy stress response, illness, or menstruation)
- Short-term (acute) or long-term (chronic) pain
- Dehydration
- Insufficient insulin
How to know if you have unstable blood sugar levels
Unstable blood sugar fluctuates between low and high blood sugar levels. Because glucose provides energy for your cells, one of the most obvious symptoms of unstable blood sugar is major changes in your energy levels throughout the day.
Symptoms correlated with low blood sugar levels may include:
- Fatigue or energy crashes
- irritability
- Confusion
- Brain fog or cognitive dysfunction
- Blurry vision
- Elevated blood pressure
- Ravenous hunger
- Headache
- Weakness
- Dizziness
- Loss of consciousness
Low blood sugar levels also prompt the nervous system to release norepinephrine (adrenaline) or acetylcholine release, causing neurogenic symptoms. The adrenaline can cause a temporary rush of energy and anxiety, whereas the acetylcholine can cause hunger.
In the short-term, high blood sugar is less dangerous than low blood sugar, so high blood sugar may be asymptomatic. This is why you have four hormones (epinephrine, norepinephrine, cortisol, glucagon, and growth hormone) that increase blood sugar and only one that decreases it.
However, long-term high blood sugar can damage your tissues and accelerate aging. Once blood sugar reaches diabetic levels, high blood sugar symptoms may include:
- Frequent urination
- Increased thirst
- Blurry vision
- Headache
- Tiredness
- Unconsciousness
- Glucose in the urine
Overall, unstable blood sugar is very unhealthy because it increases stress hormones and puts your body in a fight-or-flight mode. This can worsen stress-related conditions or conditions that tend to worsen with poor blood sugar control, such as mental health issues and hormone imbalances.
How to maintain stable blood sugar levels

Eat a Blood Sugar-Stabilizing Low Glycemic Impact Diet
Nutrition is the most important part of stabilizing blood sugar. The low glycemic impact diet is designed to stabilize blood sugar by considering the glycemic index and glycemic load.
The glycemic index (GI) rates carbohydrate-containing foods based on how fast the food that contains 50 grams of carbohydrate raises blood glucose levels over two hours. The rate of glucose rise from the food is compared to 50 grams of pure glucose or carbohydrate in white bread. This allows for the ranking of carbohydrate-rich foods in terms of their impact on your blood glucose levels.
The glycemic load (GL) is how much carbohydrate is in the food.
The glycemic load is divided into three categories:
- Low (below 10)
- Intermediate (from 11 to 19)
- High (above 20)
A low-glycemic impact diet takes into account both GI and GL. You can eat any low-GL foods, but those with a high GL should be low in GI so as not to disrupt the blood sugar.
Carbohydrates that are harder to digest, such as vegetables, have a lower GI. By consuming low-GI foods, the rate of insulin secretion tends to be lower. In terms of insulin response, not all carbohydrates are equal. Low-GI and low-GL foods stabilize blood sugar.
Examples of the Glycemic index (GI) of carbohydrate-rich foods and their glycemic
load (GL) for 100g of food; GI below/equal to 50:
- Plain yogurt with no sugar GI=14, GL=2
- Peanut butter GI=22, GL= 5
- Low-fat milk GI=32, GL=2
- Soy milk GI=36, GL=3
- Strawberries GI=40, GL=3
- Chocolate cake GI=40, GL= 20
- Oatmeal GI=49, GL= 36
- Banana GI=54, GL= 13
- Sweet potato GI=61, GL= 14
- French fries GI=75, GL= 19
- Wheat bread without gluten GI=85, GL= 43
Low-GI foods include legumes. Milk products and certain fruits have low GIs.
Most potato products, bread, and breakfast cereals have high GIs, which are frequently higher than those of sucrose (table sugar). The GI range is most emphasized in starchy products, but fruits may also differ, as noted above.
Except for white potatoes, most vegetables, fruits, intact whole grains, and legumes have lower GI rankings. More refined and processed foods, like white bread, have a high GI ranking
Benefits of a low-glycemic impact diet include
- Reduces the risk of heart health issues
- Increases satiety and reduces food intake
- Enhances post-meal glucose and lipid metabolism
- Lowers daytime blood sugar fluctuations
Clinical studies show that low-glycemic impact diets reduce body weight, body fat, blood glucose, and blood lipids. Also, lower glycemic impact foods tend to be higher in fiber and protein, so the diet increases satiety and reduces hunger.
Although the original low-glycemic impact diet relied on one glycemic impact table for everyone, recent studies suggest that the blood sugar response to each food may be very individual. This new information suggests that your microbiome, lifestyle choices, blood sugar response, and genetics control the blood sugar of each food. For example, one person could have stable blood sugar in response to bananas, whereas another person would have notable blood sugar fluctuations from it
Therefore, when Matt and Wade coach their clients, they advise each client to use continuous glucose monitoring (see below) to determine the foods best stabilizing their blood sugar.
Exercising More Often

Exercise promotes muscle insulin sensitivity, which is important for blood sugar control and insulin sensitivity.
You may not even need a lot—as little as 7.5 minutes of high-intensity exercise per week was sufficient to help control blood glucose and improve insulin sensitivity in a 2013 study. Although all kinds of exercise are beneficial, high-intensity exercise is better at stabilizing blood sugar than its low-intensity counterparts
High-intensity interval training entails repeating the exercise for at least 30 seconds to several minutes with rest intervals in between. It should be performed with maximum effort, ranging from 8 to 10 out of 10-point exertion scale. Here, your heart rate and breathing will be so fast you can’t carry on a conversation.
Low-intensity exercise is defined by less than 7 out of 10 rates of perceived exertion (the amount of work you feel your body doing) and a heart rate that is less than 70% of your maximum heart rate. At this intensity, you should be able to carry on a conversation.
You can calculate the percentage of your maximum heart rate by subtracting your age from the number 220 (i.e., a 50-year-old person would calculate 220-50 for a maximum heart rate of 170).
Having more muscle mass also improves blood sugar control, so consider resistance training and muscle building
Find out if HIIT is better than steady-state cardio for fat loss.
Taking ice baths
Cold exposure can increase energy expenditure as well as the use of glucose. Repeated exposures can reduce fasting glucose and insulin levels.
Because your body loses heat more readily in water than in the air, the water feels much colder at 20oC (68oF) than when surrounded by air at 20oC. Immersion in 20°C cold water doubles the metabolic rate during the bath and is quadrupled at 14 °C (57.2). This suggests increased metabolic rates by using blood glucose. Exposure to 14-15 °C promotes an approximately 43% increase in blood sugar control.
Practicing stress management

An unhealthy psychological stress response impairs glucose metabolism. Stress hormones such as cortisol and adrenaline raise glucose and thus glycosylated hemoglobin (HbA1C).
The spikes in blood glucose from unhealthy stress response require the pancreas to produce insulin, so this can cause insulin resistance as much as food can. As a result, stress can contribute to blood sugar-related issues, including high blood sugar and heart health challenges.
However, it’s not the external circumstances that throw off your blood sugar but how your body perceives the stress. Changing unhealthy stress response and using self-care practices to calm down during these times can improve your blood sugar stability.
Making sure to get enough sleep
We spend roughly one-third of our lives sleeping. Significant changes in glucose tolerance occur during sleep and influence glucose utilization. Chronic sleep disturbances impair glucose metabolism and increase insulin.
Sleep duration and quality significantly impact glucose homeostasis, including glucose intolerance and insulin resistance. Therefore, getting enough uninterrupted sleep and maximizing sleep quality is important to stabilizing your blood sugar.
Maintaining a healthy weight
Maintaining a healthy weight, eating a nutritious and well-balanced diet, exercising regularly, and getting at least eight hours of sleep are all important factors in achieving stable blood sugar levels.
Excessive weight gain is linked to a higher risk of developing blood sugar irregularities. Adipose (fat) tissue in over weight people releases factors that contribute to the development of these irregularities. The inability to regulate blood glucose levels occurs when blood sugar irregularities is combined with the dysfunction of β-cells (cells that release insulin).
Strengthening your gut lining
The microbiota in the gut is linked to a variety of metabolic issues. They also influence body weight and blood sugar control.
Environmental factors (like diet) can change your microbial composition and metabolism in a way that may cause metabolic challenges. Overgrowth of bad bacteria and a leaky gut can allow the bacteria toxins into the bloodstream, leading to metabolic endotoxemia or an intoxicated state from the toxins.
A leaky gut increases the variation in post-meal blood glucose levels, in turn negatively affecting metabolic control—which enables us to respond to signals by regulating enzymes in a pathway to increase or decrease their response to signals.
Factors that cause leaky gut or increase intestinal permeability include:
- Sugar and sodium chloride
- High-fat meals, especially saturated fats
- Low-fiber and low-polyphenol diets
A leaky gut may cause damaged pancreatic β-cells (which produce insulin) to produce more cytokines, resulting in insulin resistance
Microbiome Breakthrough is an innovative synbiotic blend that promotes a healthier gut barrier and immune balance in various ways. Probiotics and prebiotics improve the microbiome composition. Probiotics ferment prebiotics, producing favorable postbiotics like short-chain fatty acids (SCFAs).
SCFAs strengthen the gut barrier, stimulate the immune-balancing regulatory T cells, and inhibit bad bacteria and fungal growth.
In addition, IgYmax helps escort out the bad bacteria and pathogens, making more room for the good ones. A clinical study found that it improved the microbiome composition and balanced the gut inflammatory response.
Overall, Microbiome Breakthrough is a synergistic science-based formula that supports your microbiome and promotes good bacteria in the gut, which may improve metabolism. It can also support healthy insulin sensitivity and weight loss along with a diet and exercise program.
Other supplements that support stable blood sugar levels

Bee Propolis
Propolis is resin-like substances that bees collect from various plants. They have antioxidant, anti-inflammatory, antibacterial, antifungal, lipid-balancing, and blood sugar-balancing properties.
Having persistently high blood sugar increases oxidative stress, which impairs β-cell (pancreatic cell that produces insulin) function and reduces your insulin sensitivity. Because of its antioxidant properties, propolis may be able to improve metabolic disorders. The effect of propolis depends on the dose, country, environmental conditions of the collection site, season, and vegetation.
Because of its antioxidant properties, propolis may be able to improve metabolic disorders. In rats, propolis increased insulin sensitivity. In animal models, propolis improved insulin sensitivity, blood sugar, HbA1c, and insulin levels.
In diabetic rats, encapsulated propolis enhanced insulin sensitivity.
In a different 8-week animal study, rats were given propolis supplements ranging from 100 to 300 mg/kg, which improved insulin resistance by decreasing insulin plasma levels.
Bitter melon
Momordica charantia, also known as bitter melon, karela, balsam pear, or bitter gourd, is well known for its lipid-lowering effects. The benefits include pancreatic β-cell regeneration, insulin release, and combating the major issue of insulin resistance.
Bitter melon is rich in vitamins, antioxidants, minerals, and bioactive compounds. The plant and fruit extracts(charantin and insulin-like peptides) have blood sugar-lowering effects.
Berberine
Berberine is a major active component extracted from Chinese herbs, such as Coptis chinensis and Phellodendron amurense. Berberine is associated with a blood sugar-lowering effect
Berberine works mainly by increasing insulin secretion and insulin receptors, improving insulin sensitivity.
Cinnulin PF
Cinnulin PF is a specific water extract of cinnamon. Cinnamon extracts stimulate glucose uptake, acting as an insulin sensitizer. Cinnamon also has antioxidant properties that may benefit hormone signaling.
Cinnulin PF supplementation supports blood sugar stability. Combining Cinnulin PF with a healthy diet and exercise may result in even better health benefits. Cinnamon extracts may reduce oxidative stress, which is important because oxidative stress reduces your insulin sensitivity
Chromium
Chromium is a vital mineral that aids in the regulation of insulin. It is necessary for insulin activity and glucose metabolism. Chromium promotes glucose tolerance by lowering insulin resistance and facilitating insulin signaling.
The amount of chromium present in the body decreases with age , so, chromium supplementation may improve insulin sensitivity throughout the body.
Innoslim
Astragalus membranaceus and Panax notoginseng both have a long history of use. InnoSlim is a mixture of highly purified root extracts from the two plants with specific components that aid in weight management and metabolic regulation, when combined with a healthy diet and exercise regimen.
Benfotiamine
Benfotiamine is a fat‐soluble thiamine (vitamin B1)derivative. It also has antioxidant properties. Benfotiamine may be able to prevent a variety of health problems by reducing oxidative stress. Apart from reducing oxidative stress, benfotiamine also increases glucose uptake.
The main property of benfotiamine is blood sugar level normalization. Benfotiamine can slow or stop the progression of many severe complications associated with prolonged high blood sugar.
Alpha Lipoic Acid
Alpha-lipoic acid is an all-natural compound with antioxidant and anti-inflammatory properties. It has many beneficial functions for our health and our wellbeing. Examples include: anti-oxidation, blood sugar regulation, and recycling antioxidants like glutathione and vitamins C and E.
Insulin therapy and alpha-lipoic acid promote normalization of blood sugar, reduce oxidative stress, and improve β-cell function and insulin sensitivity. Alpha-lipoic acid aids in the defense against oxidative stress by boosting the synthesis of anti-oxidants such as glutathione—the body’s most abundant antioxidants.
Gymnema Sylvestre
Gymnema Sylvestre is an ancient medicinal plant used in Ayurvedic medicine, and is a widely used hypoglycemic (blood sugar-lowering), hypolipidemic (lipid-lowering), antiviral (effective against viruses), diuretic (increased urination), antibiotic, and weight loss supplement.
Its phytochemicals, which include gurmarin, gymnemic acid, and gymnema saponins, have blood sugar-lowering activity.
Banaba leaf

Banaba (Lagerstroemia speciosa) has strong blood sugar-balancing properties and exerts these effects due to the presence of corosolic acid.
In a diabetes management study, corosolic acid increased cellular uptake of glucose and improved insulin sensitivity.
Berberine Breakthrough contains a synergistic combination of these blood sugar-balancing ingredients, and we have found that it promotes blood sugar balance in clinical trials.
Magnesium
Magnesium (Mg) is the body’s fourth most abundant cation and plays an important role in many bodily functions. Low Mg intake and serum Mg deficiency are linked to an increased risk of the development of metabolic diseases.
Magnesium is needed for proper glucose utilization as well as insulin signaling. Magnesium supplementation also supports healthy blood sugar and insulin-sensitivity.
If you are considering magnesium supplementation, try out Magnesium Breakthrough. It is the only magnesium supplement on the market that gives you seven highly-absorbed forms of magnesium and only two capsules are needed to get your daily dose of elemental magnesium (500 mg), while most other brands only have 30 to 80 mg of elemental magnesium. Magnesium is not only beneficial for stabilizing blood sugar levels, but also for promoting a healthy stress response, restorative sleep, immune system readiness, and strong bones.
How to know if you have stable blood sugar
If you have stable blood sugar, you feel even-keeled, and your energy levels won’t fluctuate much throughout the day. Rather, you’ll constantly feel energized and in a good mood. Hunger won’t feel excessive, and meals will remove hunger without making you tired. Your mind will be clear, and you’ll feel your brain functioning optimally.
But ideally, it’s better to correlate your symptoms with tests, such as those that measure blood sugar levels.
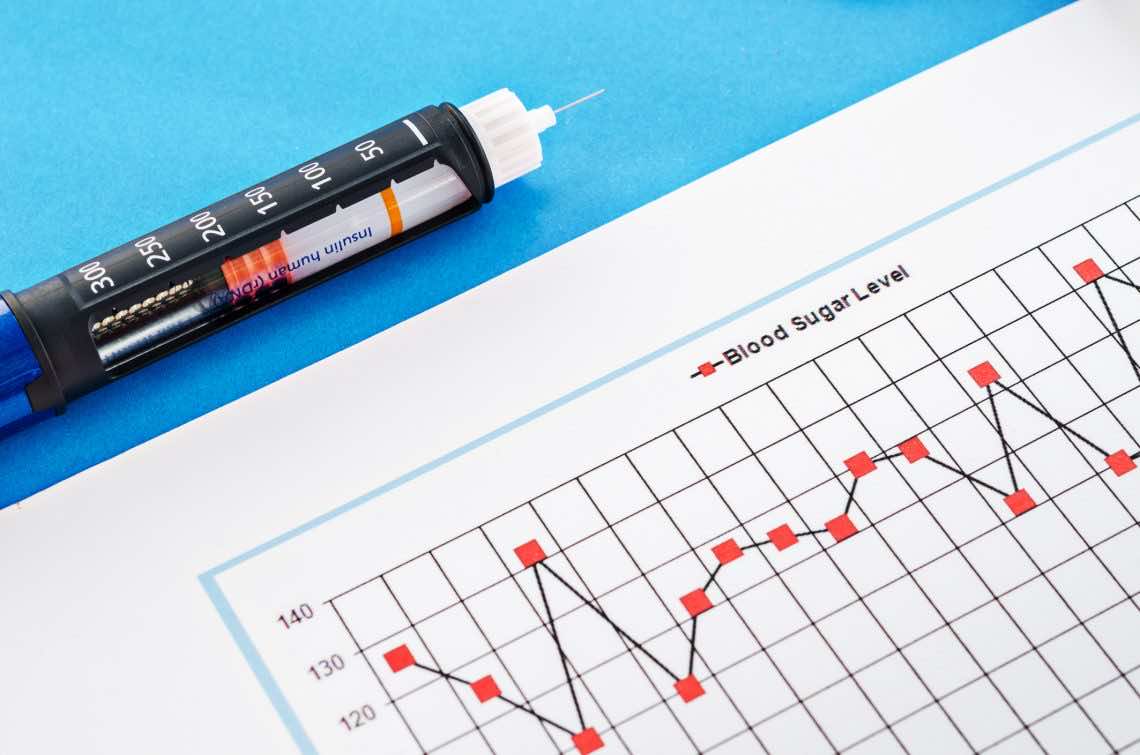
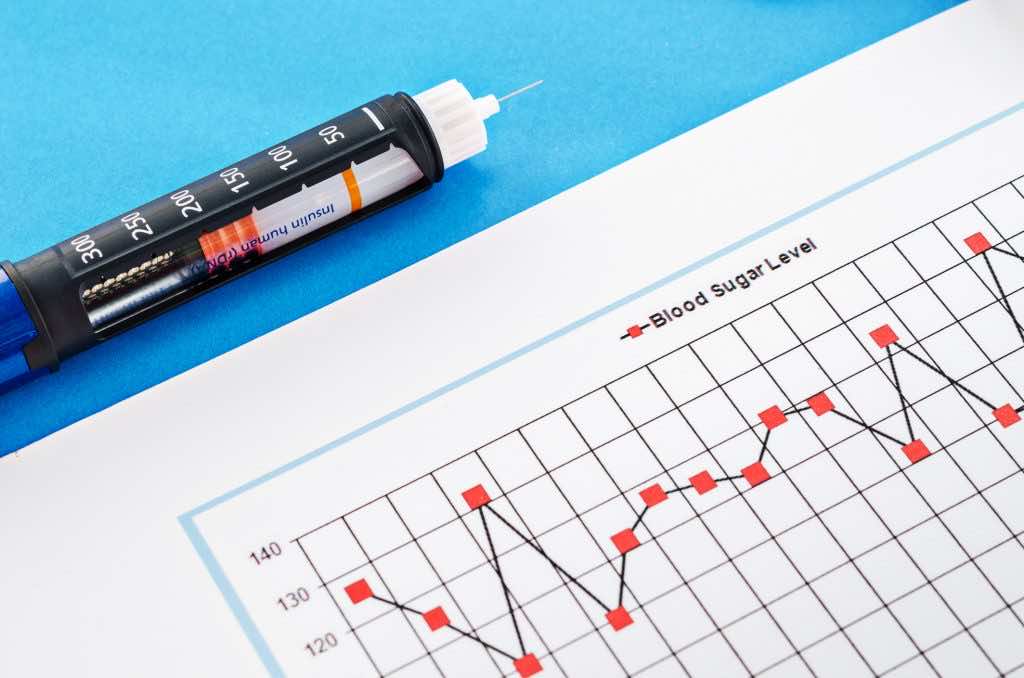
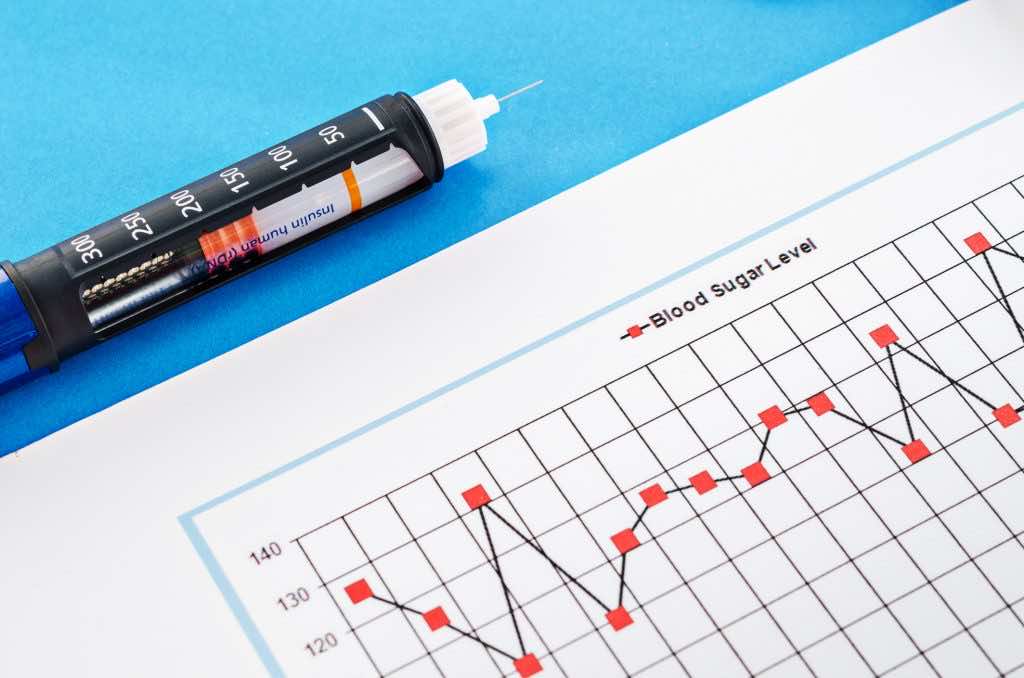
How to monitor and test for blood sugar levels

Blood sugar monitoring allows you to observe changes in your blood sugar levels in response to diet, exercise,medications, and stressors. These things can all cause blood sugar fluctuations.
Currently, there are four options to monitor your blood sugar level: glucometer, continuous glucose monitoring, fasting blood sugar, and hemoglobin A1c tests.
Glucometer
A glucometer is a device you buy at the pharmacy along with the test strips. To test your blood glucose, you prick your finger with a lancet and put a droplet of blood into the glucometer strip. Then, the glucometer reads your blood sugar.
While a glucometer is a convenient option to test your blood glucose at home, it is less accurate than a blood test you get at the doctor’s office.
Continuous glucose monitoring (CGM)
Continuous interstitial fluid glucose monitoring involves placing a disposable and water-resistant sensor on the backside of your upper arm or onto your stomach/abdomen. The sensor can stay on your body for 3 to 14 days. By scanning the sensor with a reader, you obtain your results. The results show your glucose levels over the last eight hours.
Instead of testing glucose directly in the blood, it measures the glucose in the fluid around your cells (interstitial fluid), which correlates with your blood glucose.
Normal fasting blood sugar concentrations are between 63-100 mg/dL. Postprandial blood glucose (glucose levels after a meal) goes up to 120-140.
Blood sugar increases after a meal and then quickly returns within the normal range. Having the interstitial glucose measured on a continuous basis or every few minutes allows you to see the effects of different meals, stressors, and exercises on your blood glucose.
Fasting blood sugar test

This test involves a blood draw in the doctor’s office or at the lab after a 10-14 hour fast, during which only water consumption is allowed. Because caffeine and nicotine may increase your blood sugar, avoid coffee or smoking before your blood draws. The reference range for the fasting blood sugar test is from 70-99 mg/dL.
The normal range for fasting blood sugar is 60-140 mg/dL, although many functional medicine and anti-aging doctors consider the range 70-85 mg/dL to be the healthiest optimal range. Typically, a lower number within the range correlates with better blood sugar stability.
Keep in mind, however, if you’re on a low-carb or ketogenic diet, your fasting blood sugar will be elevated, but this doesn’t reflect poor blood sugar control. Therefore, your doctor may look at other tests, such as hemoglobin A1c, and correlate the results with your symptoms and history.
Hemoglobin A1C (HbA1c) test
Hemoglobin is a protein found in red blood cells. Glucose in the blood binds to the hemoglobin protein, creating Hemoglobin A1c. For an HbA1c test to be considered normal, the value must be less than 5.7%.
The higher your blood glucose is for two to three months, the more HbA1c you will have.
Getting an HbA1c (A1c) test at least twice a year is a good way to determine your average blood sugar for the previous two to three months. The hemoglobin A1c (HbA1c) test determines a person’s glucose control. Aside from blood sugar, HbA1c is also determined by genetics and the lifespan of your white blood cells.
HbA1c is a suitable and secure indicator of blood sugar control and a good predictor of diabetes-related complications in people who do not have diabetes.
Conclusion
Having healthy and stable blood sugar is vital for health and performance. You can achieve it through a healthy lifestyle, eating a low glycemic impact diet, exercising, sleeping well, and managing stress. If you enjoy a high-carb meal or are in a pinch with an impending blood sugar crash, supplements that contain blood sugar-balancing ingredients, such as Berberine Breakthrough, can promote healthy blood sugar levels and help improve irregularities in the blood sugar.
References
- Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. J Clin Invest. 2016;126(1):12-22.
- Wilcox G. Insulin and insulin resistance. Clin Biochem Rev. 2005;26(2):19-39.
- Freeman AM, Pennings N. Insulin Resistance. In: StatPearls. StatPearls Publishing; 2021.
- Good to know: Factors affecting blood glucose. Clin Diabetes. 2018;36(2):202.
- Mathew P, Thoppil D. Hypoglycemia. In: StatPearls. StatPearls Publishing; 2021.
- Evans Kreider K, Pereira K, Padilla BI. Practical approaches to diagnosing, treating and preventing hypoglycemia in diabetes. Diabetes Ther. 2017;8(6):1427-1435.
- Mathew TK, Tadi P. Blood Glucose Monitoring. In: StatPearls. StatPearls Publishing; 2021.
- Cowart SL, Stachura ME. Glucosuria. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. Butterworths; 2011.
- Nguyen HT, Arcury TA, Grzywacz JG, et al. The association of mental conditions with blood glucose levels in older adults with diabetes. Aging Ment Health. 2012;16(8):950-957.
- Gambineri A, Pelusi C. Sex hormones, obesity and type 2 diabetes: is there a link? Endocr Connect. 2019;8(1):R1-R9.
- Wolever TM. The glycemic index. World Rev Nutr Diet. 1990;62:120-185.
- Rizkalla SW, Bellisle F, Slama G. Health benefits of low glycaemic index foods, such as pulses, in diabetic patients and healthy individuals. Br J Nutr. 2002;88 Suppl 3(S3):S255-62.
- Zafar MI, Mills KE, Zheng J, et al. Low-glycemic index diets as an intervention for diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2019;110(4):891-902.
- Eleazu CO. The concept of low glycemic index and glycemic load foods as panacea for type 2 diabetes mellitus; prospects, challenges and solutions. Afr Health Sci. 2016;16(2):468-479.
- Bittencourt, J. The Power of Carbohydrates, Proteins, and Lipids: How To Make Wise Choices In Diet And Nutrition. 2018. CreateSpace Independent Publishing Platform.
- Björck I, Liljeberg H, Östman E. Low glycaemic-index foods. Br J Nutr. 2000;83(S1):S149-S155.
- Rovner AJ, Nansel TR, Gellar L. The effect of a low-glycemic diet vs a standard diet on blood glucose levels and macronutrient intake in children with type 1 diabetes. J Am Diet Assoc. 2009;109(2):303-307.
- Zafar MI, Mills KE, Zheng J, Peng MM, Ye X, Chen LL. Low glycaemic index diets as an intervention for obesity: a systematic review and meta-analysis: Low GI diets for obesity. Obes Rev. 2019;20(2):290-315.
- Zeevi D, Korem T, Zmora N, et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163(5):1079-1094.
- Suh S-H, Paik I-Y, Jacobs K. Regulation of blood glucose homeostasis during prolonged exercise. Mol Cells. 2007;23(3):272-279.
- Adams OP. The impact of brief high-intensity exercise on blood glucose levels. Diabetes Metab Syndr Obes. 2013;6:113-122.
- Shiraev T, Barclay G. Evidence based exercise – clinical benefits of high intensity interval training. Aust Fam Physician. 2012;41(12):960-962.
- Target heart rate and estimated maximum heart rate. Cdc.gov. Published October 14, 2020.https://www.cdc.gov/physicalactivity/basics/measuring/heartrate.htm Accessed September 15, 2021.
- Eston R. Use of ratings of perceived exertion in sports. Int J Sports Physiol Perform. 2012;7(2):175-182.
- Lee J, Kim D, Kim C. Resistance training for glycemic control, muscular strength, and lean body mass in old type 2 diabetic patients: A meta-analysis. Diabetes Ther. 2017;8(3):459-473.
- Ivanova YM, Blondin DP. Examining the benefits of cold exposure as a therapeutic strategy for obesity and type 2 diabetes. J Appl Physiol. 2021;130(5):1448-1459.
- Mooventhan A, Chaudhari SS, Venugopal V. Effect of cold hip bath on blood glucose levels in patients with type 2 diabetes mellitus: A pilot study. Diabetes Metab. 2020;46(5):411-412.
- Nowotny B, Cavka M, Herder C, et al. Effects of acute psychological stress on glucose metabolism and subclinical inflammation in patients with post-traumatic stress disorder. Horm Metab Res. 2010;42(10):746-753.
- Zamani-Alavijeh F, Araban M, Koohestani HR, Karimy M. The effectiveness of stress management training on blood glucose control in patients with type 2 diabetes. Diabetol Metab Syndr. 2018;10(1):39.
- Yitshak-Sade M, Mendelson N, Novack V, Codish S, Liberty IF. The association between an increase in glucose levels and armed conflict-related stress: A population-based study. Sci Rep. 2020;10(1):1710.
- Surwit RS, Schneider MS, Feinglos MN. Stress and diabetes mellitus. Diabetes Care. 1992;15(10):1413-1422.
- Scheen AJ, Byrne MM, Plat L, Leproult R, Van Cauter E. Relationships between sleep quality and glucose regulation in normal humans. Am J Physiol. 1996;271(2 Pt 1):E261-70.
- Knutson KL. Impact of sleep and sleep loss on glucose homeostasis and appetite regulation. Sleep Med Clin. 2007;2(2):187-197.
- Xu X, Wang L, Zhang Y, et al. Effects of chronic sleep deprivation on glucose homeostasis in rats. Sleep Biol Rhythms. 2016;14(4):321-328.
- Asif M. The prevention and control the type-2 diabetes by changing lifestyle and dietary pattern. J Educ Health Promot. 2014;3(1):1.
- Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444(7121):840-846.
- Do MH, Lee E, Oh M-J, Kim Y, Park H-Y. High-glucose or -fructose diet cause changes of the gut Microbiota and metabolic disorders in mice without body weight change. Nutrients. 2018;10(6). doi:10.3390/nu10060761
- Mechanisms linking the gut microbiome and glucose metabolism. J Clin Endocrinol Metab. 2016;101(4):1445-1454.
- Fuke N, Nagata N, Suganuma H, Ota T. Regulation of gut Microbiota and metabolic endotoxemia with dietary factors. Nutrients. 2019;11(10):2277.
- Li X, Atkinson MA. The role for gut permeability in the pathogenesis of type 1 diabetes–a solid or leaky concept?: Leaky gut in type 1 diabetes. Pediatr Diabetes. 2015;16(7):485-492.
- Damci T, Nuhoglu I, Devranoglu G, Osar Z, Demir M, Ilkova H. Increased intestinal permeability as a cause of fluctuating postprandial blood glucose levels in Type 1 diabetic patients. Eur J Clin Invest. 2003;33(5):397-401.
- Metabolism Control. News-medical.net. Published November 26, 2009. Accessed September 15, 2021. https://www.news-medical.net/life-sciences/Metabolism-Control.aspx
- Pereira MT, Malik M, Nostro JA, Mahler GJ, Musselman LP. Effect of dietary additives on intestinal permeability in both Drosophila and a human cell co-culture. Dis Model Mech. 2018;11(12):dmm034520.
- Pendyala S, Walker JM, Holt PR. A high-fat diet is associated with endotoxemia that originates from the gut. Gastroenterology. 2012;142(5):1100-1101.e2.
- Krawczyk M, Maciejewska D, Ryterska K, et al. Gut permeability might be improved by dietary fiber in individuals with nonalcoholic fatty liver disease (NAFLD) undergoing weight reduction. Nutrients. 2018;10(11):1793.
- de Kort S, Keszthelyi D, Masclee AAM. Leaky gut and diabetes mellitus: what is the link?: Leaky gut in diabetes. Obes Rev. 2011;12(6):449-458.
- Markowiak P, Śliżewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. 2017;9(9):1021.
- van der Beek CM, Dejong CHC, Troost FJ, Masclee AAM, Lenaerts K. Role of short-chain fatty acids in colonic inflammation, carcinogenesis, and mucosal protection and healing. Nutr Rev. 2017;75(4):286-305.
- Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Troost FJ, Brummer R-J. Review article: the role of butyrate on colonic function: review: role of butyrate on colonic function. Aliment Pharmacol Ther. 2008;27(2):104-119.
- Ke X, Walker A, Haange SB, et al. Synbiotic-driven improvement of metabolic disturbances is associated with changes in the gut microbiome in diet-induced obese mice. Mol Metab. 2019;22:96-109. doi:10.1016/j.molmet.2019.01.012
- Horvath A, Leber B, Feldbacher N, et al. Effects of a multispecies synbiotic on glucose metabolism, lipid marker, gut microbiome composition, gut permeability, and quality of life in diabesity: a randomized, double-blind, placebo-controlled pilot study. Eur J Nutr. 2020;59(7):2969-2983. doi:10.1007/s00394-019-02135-w
- IgY Max increases beneficial flora and improves gut integrity. Nutraceuticalbusinessreview.com. Accessed September 16, 2021. https://nutraceuticalbusinessreview.com/news/article_page/IgY_Max_increases_beneficial_flora_and_improves_gut_integrity/119301
- Al-Hariri MT. Propolis and its direct and indirect hypoglycemic effect. J Family Community Med. 2011;18(3):152-154.
- Zakerkish M, Jenabi M, Zaeemzadeh N, Hemmati AA, Neisi N. The effect of Iranian Propolis on glucose metabolism, lipid profile, insulin resistance, renal function and inflammatory biomarkers in patients with type 2 diabetes mellitus: A randomized double-blind clinical trial. Sci Rep. 2019;9(1):7289.
- Pahlavani N, Malekahmadi M, Firouzi S, et al. Molecular and cellular mechanisms of the effects of Propolis in inflammation, oxidative stress and glycemic control in chronic diseases. Nutr Metab (Lond). 2020;17(1):65.
- Zamami Y, Takatori S, Koyama T, et al. Effect of propolis on insulin resistance in fructose-drinking rats. Yakugaku Zasshi. 2007;127(12):2065-2073.
- Joseph B, Jini D. Antidiabetic effects of Momordica charantia (bitter melon) and its medicinal potency. Asian Pac J Trop Dis. 2013;3(2):93-102.
- Alam MA, Uddin R, Subhan N, Rahman MM, Jain P, Reza HM. Beneficial role of bitter melon supplementation in obesity and related complications in metabolic syndrome. J Lipids. 2015;2015:496169.
- Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57(5):712-717.
- Cao C, Su M. Effects of berberine on glucose-lipid metabolism, inflammatory factors and insulin resistance in patients with metabolic syndrome. Exp Ther Med. 2019;17(4):3009-3014.
- Liang Y, Xu X, Yin M, et al. Effects of berberine on blood glucose in patients with type 2 diabetes mellitus: a systematic literature review and a meta-analysis. Endocr J. 2019;66(1):51-63.
- Ziegenfuss TN, Hofheins JE, Mendel RW, Landis J, Anderson RA. Effects of a water-soluble cinnamon extract on body composition and features of the metabolic syndrome in pre-diabetic men and women. J Int Soc Sports Nutr. 2006;3(2):45-53.
- Crawford P, Thai C, Obholz J, et al. Assessment of the effeCt of lIfestyle iNtervention plus water-soluble ciNnAMon extract On loweriNg blood glucose in pre-diabetics, a randomized, double-blind, multicenter, placebo controlled trial: study protocol for a randomized controlled trial. Trials. 2016;17(1):9.
- Roussel A-M, Hininger I, Benaraba R, Ziegenfuss TN, Anderson RA. Antioxidant effects of a cinnamon extract in people with impaired fasting glucose that are overweight or obese. J Am Coll Nutr. 2009;28(1):16-21.
- A scientific review: the role of chromium in insulin resistance. Diabetes Educ. 2004;Suppl:2-14.
- Talab AT, Abdollahzad H, Nachvak SM, et al. Effects of chromium picolinate supplementation on cardiometabolic biomarkers in patients with type 2 diabetes mellitus: A randomized clinical trial. Clin Nutr Res. 2020;9(2):97.
- Ali A, Ma Y, Reynolds J, Wise JP Sr, Inzucchi SE, Katz DL. Chromium effects on glucose tolerance and insulin sensitivity in persons at risk for diabetes mellitus. Endocr Pract. 2011;17(1):16-25.
- Sharma S, Agrawal RP, Choudhary M, Jain S, Goyal S, Agarwal V. Beneficial effect of chromium supplementation on glucose, HbA1C and lipid variables in individuals with newly onset type-2 diabetes. J Trace Elem Med Biol. 2011;25(3):149-153.
- Murbach TS, Glávits R, Endres JR, et al. Toxicological Evaluation of a Mixture of Astragalus membranaceus and Panax notoginseng Root Extracts (InnoSlim®). J Toxicol. 2019;2019:5723851.
- Sohn SB, Kim TY, Kim HU, Park JM, Lee SY. Metabolic Control. In: Comprehensive Biotechnology. Elsevier; 2011:853-861.
- Chakrabarti R, Chen M, Liu W, Chen S. Preventive effects of benfotiamine in chronic diabetic complications: Benfotiamine in diabetic complications. J Diabetes Investig. 2011;2(2):123-131.
- Fraser DA, Hessvik NP, Nikolić N, et al. Benfotiamine increases glucose oxidation and downregulates NADPH oxidase 4 expression in cultured human myotubes exposed to both normal and high glucose concentrations. Genes Nutr. 2012;7(3):459-469.
- Balakumar P, Rohilla A, Krishan P, Solairaj P, Thangathirupathi A. The multifaceted therapeutic potential of benfotiamine. Pharmacol Res. 2010;61(6):482-488.
- Ebada MA, Fayed N, Fayed L, et al. Efficacy of alpha-lipoic acid in the management of diabetes mellitus: A systematic review and meta-analysis. Iran J Pharm Res. 2019;18(4):2144-2156.
- Poh ZX, Goh KP. A current update on the use of alpha lipoic acid in the management of type 2 diabetes mellitus. Endocr Metab Immune Disord Drug Targets. 2009;9(4):392-398.
- Zuñiga LY, González-Ortiz M, Martínez-Abundis E. Effect of Gymnema sylvestre administration on metabolic syndrome, insulin sensitivity, and insulin secretion. J Med Food. 2017;20(8):750-754.
- Khan F, Sarker MMR, Ming LC, et al. Comprehensive review on phytochemicals, pharmacological and clinical potentials of Gymnema sylvestre. Front Pharmacol. 2019;10:1223.
- Miura T, Takagi S, Ishida T. Management of diabetes and its complications with Banaba (Lagerstroemia speciosa L.) and corosolic acid. Evid Based Complement Alternat Med. 2012;2012:871495.
- Veronese N, Watutantrige-Fernando S, Luchini C, et al. Effect of magnesium supplementation on glucose metabolism in people with or at risk of diabetes: a systematic review and meta-analysis of double-blind randomized controlled trials. Eur J Clin Nutr. 2016;70(12):1354-1359.
- Takaya J, Higashino H, Kobayashi Y. Intracellular magnesium and insulin resistance. Magnes Res. 2004;17(2):126-136.
- Mathew TK, Tadi P. Blood Glucose Monitoring. [Updated 2021 Aug 11]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555976/
- Güemes M, Rahman SA, Hussain K. What is a normal blood glucose? Arch Dis Child. 2016;101(6):569-574.
- Nakrani MN, Wineland RH, Anjum F. Physiology, Glucose Metabolism. In: StatPearls. StatPearls Publishing; 2021.
- Glucose Tests. Labcorp.com. Accessed September 16, 2021. https://www.labcorp.com/help/patient-test-info/glucose-tests
- Eyth E, Naik R. Hemoglobin A1C. In: StatPearls. StatPearls Publishing; 2021.
- Wheeler E, Leong A, Liu C-T, et al. Impact of common genetic determinants of Hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: A transethnic genome-wide meta-analysis. PLoS Med. 2017;14(9):e1002383.
- Leong A, Wheeler E. Genetics of HbA1c: a case study in clinical translation. Curr Opin Genet Dev. 2018;50:79-85.
