Leaky Gut and Weight Gain
Leaky Gut and Weight Gain
What Are Leaky Gut And Metabolic Endotoxemia?
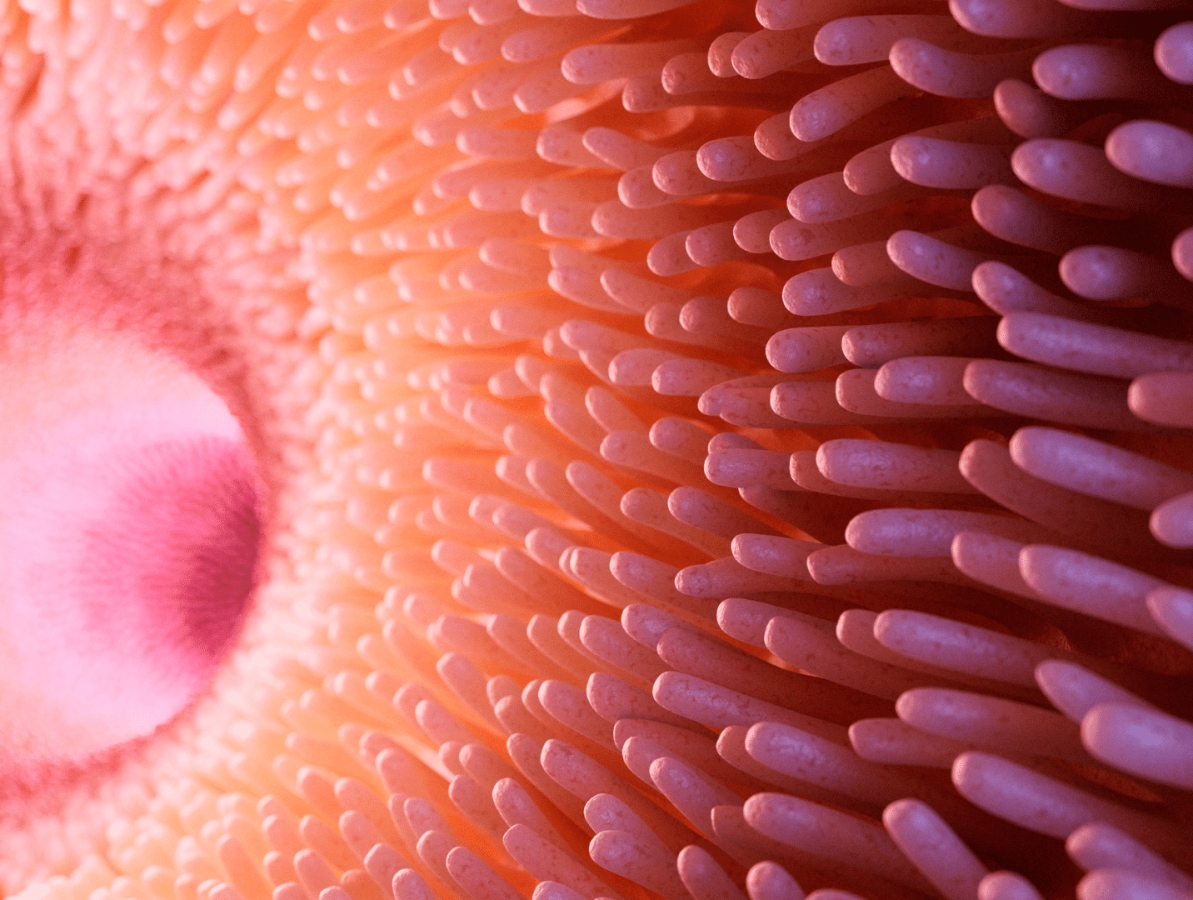
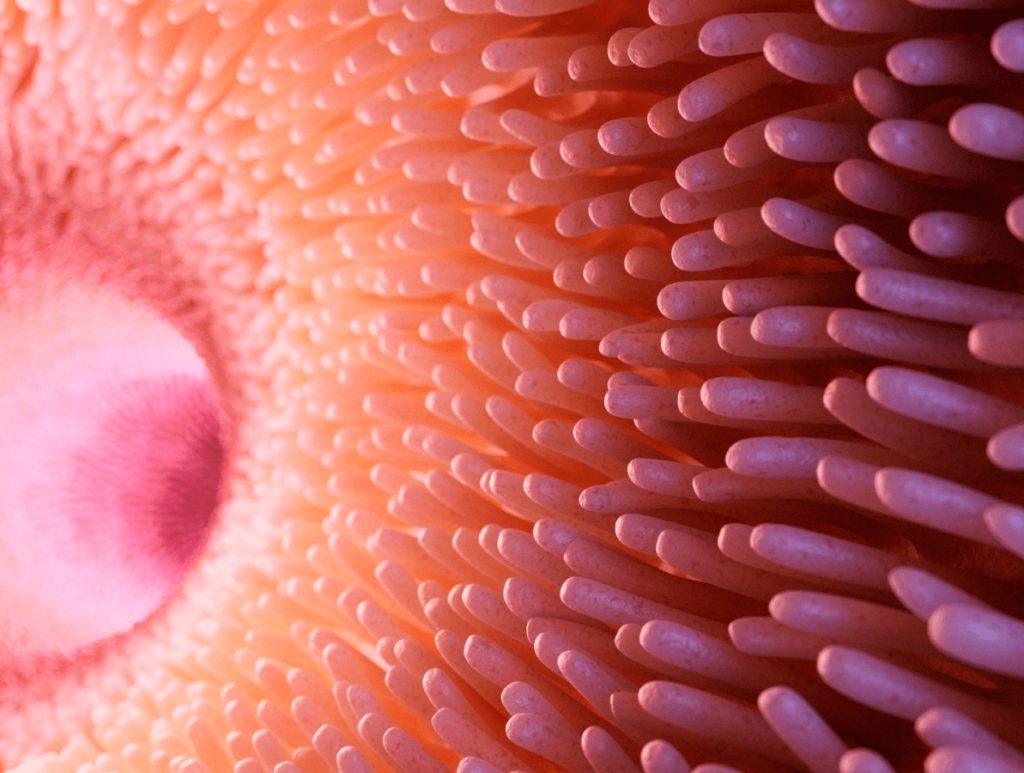
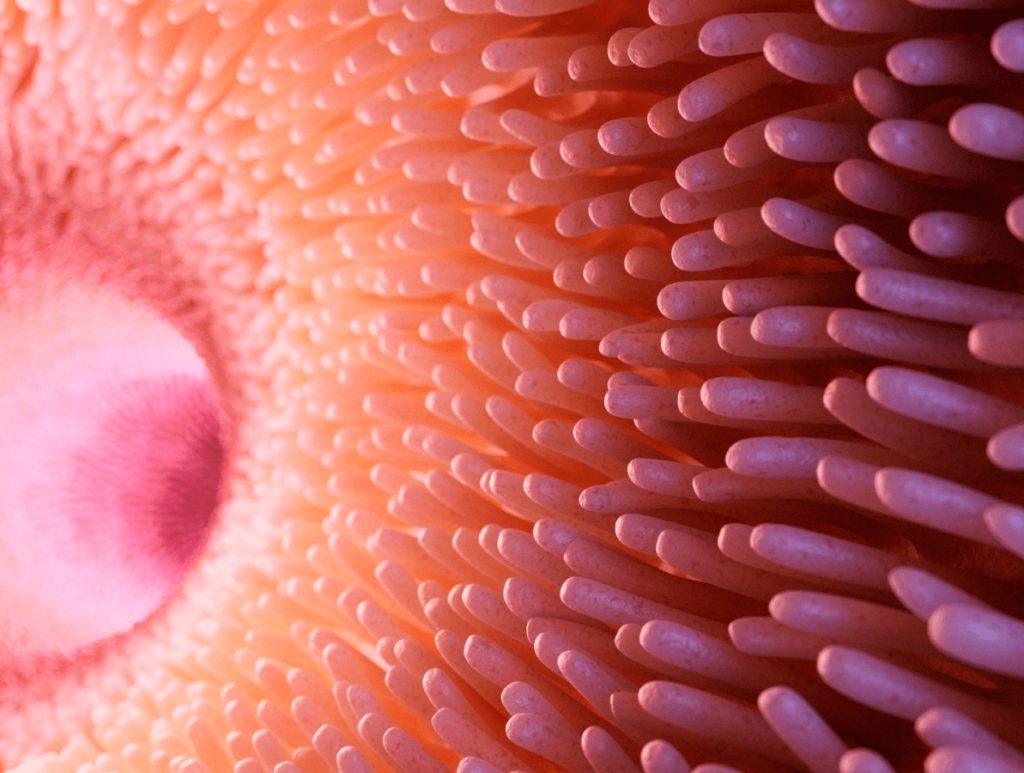
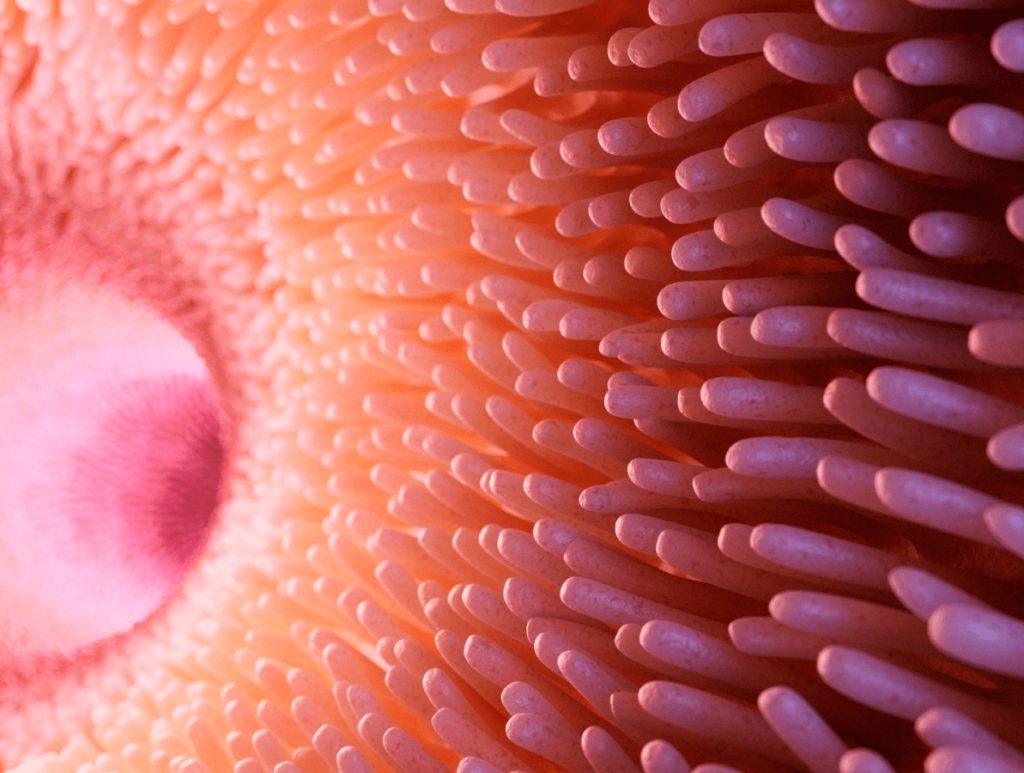
Your gut barrier comprises of a single cell layer and a mucus layer that covers it. This barrier separates your gut content, including food and microbes, from the rest of your body. When your gut barrier opens up and exposes your gut content to the immune system, you have a leaky gut.
Many things can open up your gut barrier, such as:
- Stress
- Gluten
- Head injuries
- High-fat meals
Metabolic endotoxemia, or the state of intoxication from a bacterial toxin, can happen due to leaky gut. Specifically, lipopolysaccharides (LPS), a toxic component found in Gram-negative bacteria, are the most problematic.
Large doses of LPS in your blood can lead to a life-threatening septic shock. Whereas low doses of LPS can cause chronic low-grade inflammation. The LPS activates toll-like receptors throughout the body and turns on your cells’ inflammatory response.
While metabolic endotoxemia sounds very bad, it’s very common– everyone has some degree of it. In fact, blood LPS levels go up with age which partly explains why inflammation increases with age. Whether you want to maximize aesthetics, performance, or healthspan, it’s essential to learn how to minimize metabolic endotoxemia by improving your gut health.
How Leaky Gut And Metabolic Endotoxemia Are Linked To Weight Gain And Other Health Risks
Leaky gut and the worst-case scenario of metabolic endotoxemia can cause a world of other health issues. These various health conditions can stem from the inflammation caused by LPS getting into your bloodstream.
Obesity
People with obesity suffer from chronic inflammation. In a controlled study of 1,347 diabetic subjects, the obese subjects were more likely to have higher LPS. When LPS gets into your bloodstream due to leaky gut, it can lead to obesity through various mechanisms:
- It activates your fat cells by binding to the fat cells’ Toll-like receptors. LPS then causes inflammation of the fat cells, whereby the fat cells swell, resulting in obesity.
- Chronic LPS exposure may also increase leptin resistance by causing inflammation and disruption of the gut-brain axis. Leptin is the hormone responsible for telling our brains when we are full. Leptin resistance can lead to intense hunger and overeating.
Insulin Resistance
When you eat, your body needs to release insulin to get blood sugar to your cells for energy. The inflammatory response that occurs when LPS is in your bloodstream can disrupt insulin receptor signaling. If the insulin response isn’t working correctly, you could end up with insulin resistance and increase your risk for diabetes.
In a study exploring the effects of LPS on insulin activity, participants consisted of twelve lean subjects, nine non-diabetic obese subjects, and ten obese subjects with type 2 diabetes. LPS was considerably higher in all obese subjects and associated with higher insulin resistance. At a muscular level, researchers also observed that higher concentrations of LPS increased the expression of inflammatory genes and led to impaired glucose transport.
Cardiovascular Risk
Both obesity and insulin resistance contribute to higher cardiovascular risk. Even more directly, LPS promotes atherosclerosis, the thickening of your arteries.
A study of 810 participants examined the link between inflammatory response and atherosclerosis. Subjects with higher rates of circulating endotoxins like LPS were more likely to have atherosclerosis. This is likely due to the body’s inflammatory response increasing arterial plaque formation.
LDL Cholesterol
The health risks associated with metabolic endotoxemia continue to affect LDL cholesterol levels (the “bad” cholesterol linked to a higher risk of heart disease and stroke).
A meta-analysis of 7,178 subjects explored the relationship between metabolic endotoxemia and its effects on the body by examining subjects’ serum profiles. Subjects with high levels of LPS activity had high levels of LDL cholesterol and low levels of HDL cholesterol (the “good” one).
LPS And Your Brain
LPS can wreak havoc on your mental health. LPS can cross the blood-brain barrier, cause inflammation in your brain, and cause depression by inhibiting dopamine receptors.
When individuals are exposed to endotoxins in a clinical setting, they quickly experience depressive-like symptoms such as:
- Negative mood
- Sadness
- Anxiety
- Lack of energy
- Lack of feeling pleasure
Endotoxemia inflammation in the brain may also play a role in age-related cognitive decline and Alzheimer’s disease. A review of studies examining the connection between LPS and Alzheimer’s disease confirmed the presence of LPS in the brain of those with Alzheimer’s. Scientists believe that LPS and other factors lead to the amyloid plaques found in Alzheimer’s patients.
Overall, metabolic endotoxemia creates inflammation throughout your entire body and can affect any cell’s inflammation response. If you already suffer from an inflammatory disease, it can add fuel to the fire.
What Causes Metabolic Endotoxemia?
LPS is excreted in your gut as bacteria die off, and your gut bacteria constantly die off. Bacterial turnover increases during digestion, especially postprandial or after your meal. The die-off that occurs releases LPS. What you eat can increase the amount of LPS released.
High-Fat, Sugar, And Salt Diet, Especially Saturated Fat

What you eat matters when it comes to contributing to metabolic endotoxemia. Many scientists believe that the Western diet, typically high in fat, is the key link between inflammation, obesity, and most other modern lifestyle diseases.
Eating a high-fat diet can increase the toxicity of the LPS produced and the permeability of your epithelial lining, allowing LPS to pass through your intestinal wall and enter your bloodstream.
In a study of 20 healthy individuals, half ate a high-fat meal, and half ate a low-fat meal of 910 calories. Scientists took blood samples before and after the meal. Those who ate high-fat meals had increased levels of LPS in their bloodstream, and those who ate the low-fat meal had no increase in LPS levels. Eating a high-fat diet, even just one meal, increases LPS levels and your risk of endotoxemia.
Saturated fat is even worse for increasing your risk of metabolic endotoxemia. In a study of 48 healthy subjects, participants drank one of four drinks equaling 300 calories after fasting overnight:
- 75g of glucose
- 33 g of heavy whipping cream (70% saturated fat)
- Orange juice
- 300 mL of water
Researchers then collected blood samples. Compared to all of the groups, LPS increased only in the group that drank heavy whipping cream.
A diet high in sugar or salt increases your risk of metabolic endotoxemia by disrupting your gut health. Remember, everyone has LPS in their system. Only when you have a leaky gut can the LPS pass through your lining and into your bloodstream. Dysbiosis, or gut imbalance, is a major contributing factor to leaky gut.
In an animal study, a high-salt diet altered the gut composition of mice. This led to a higher ratio of Firmicutes to Bacteroidetes and lowered the amount of beneficial probiotic Lactobacillus. An additional animal study found salt-induced gut dysbiosis and inflammation of the blood vessels.
Diets high in refined sugar can also lead to dysbiosis. When you overeat sugar, the diversity of your gut bacteria diminishes, leading to gut imbalance and inflammation.
Alternative Non-Caloric Sweeteners
While a diet high in sugar can disrupt your gut, beware of the alternative. In recent years, alternative sweeteners are becoming increasingly popular, but there may be better choices for your gut.
In a controlled animal study, Wistar rats were divided into groups to examine the effects of no-calorie sweeteners like stevia and sucralose versus caloric natural sweeteners like honey and brown sugar.
The gut microbiome was least diverse in the rats that consumed non-caloric sweeteners. These groups also experienced a decrease in beneficial bacteria. The group that consumed honey had an increase in good bacteria.
Therefore, to help prevent gut dysbiosis and decrease the likelihood of metabolic endotoxemia, keep your refined sugar consumption low and stick to natural sweeteners to support your gut health rather than an unhealthy no-calorie alternative.
Lack Of Fiber And Polyphenols
If your diet lacks fiber and polyphenols, your gut isn’t getting what it needs for optimal health. Both fiber and polyphenols are prebiotics for good bacteria. Because digestive enzymes don’t break down fiber and polyphenols are poorly absorbed, they provide food for good bacteria to multiply. Making sure to give your good bacteria what they need to thrive can help prevent dysbiosis.
A meta-analysis of eleven studies examined the effects of dietary fiber on gut microbiota, LPS, and inflammatory markers. While the diet did not affect inflammatory markers, groups that ate a low-fiber diet had higher levels of LPS and less gut diversity than those eating a high-fiber diet. High LPS levels are likely due to a low-fiber diet contributing to an imbalanced gut.
Polyphenols not only protect the epithelial lining from oxidative stress but may also play a role in protein expression in the tight junctions of the intestinal wall, which can prevent permeability.
Not including these in your diet by “eating the rainbow” is a mistake that will put your gut at risk.
What Reduces/Helps With Metabolic Endotoxemia?
The solution to reducing metabolic endotoxemia is to heal your gut. If your gut is healthy, your gut lining is more likely to remain intact and prevent endotoxins from passing through and entering your bloodstream.
Note: While studies are unequivocal that probiotics and synbiotics are very beneficial, these alone are not enough to cure diseases linked to metabolic endotoxemia. You also need to eat better, exercise, and address root causes of leaky gut to fully address metabolic endotoxemia. Please also see your healthcare provider to diagnose and treat any medical conditions.
Probiotics/Synbiotics
Having a healthy gut means having more diverse and balanced gut bacteria. Adding the right probiotics to your daily routine can help treat and prevent metabolic endotoxemia. Certain probiotics are scientifically proven to decrease LPS levels.
Lactobacillus rhamnosus GG (LGG) has positive effects on metabolic endotoxemia. In a 12-week placebo-controlled study of 44 subjects, scientists gave subjects 1.6 billion CFUs of LGG in addition to a calorie-restricted diet. While all subjects experienced some weight loss, those that took LGG had decreased levels of LPS and improved cardiovascular risk factors.
Other probiotics have similar effects on LPS and additional metabolic benefits. Bifidobacterium breve also increases HDL cholesterol levels, which boosts overall heart health.
A meta-analysis of the effects of probiotics on weight loss specifically highlights lactobacillus gasseri (L. gasseri) for its impact on body weight. However, while one strain may cause weight loss, another strain of the same probiotic may cause weight gain.
Another probiotic, Lactiplantibacillus plantarum (formerly Lactobacillus plantarum or L. plantarum), can support overall gut health. A review of L. plantarum examined its wide range of benefits. L. plantarum:
- Thrives in the harsh acidic environment of the human gut.
- Adheres well to the mucosal lining of the intestines, further creating a barrier to protect it from invaders
- Strengthens the gut barrier
- Inhibits suboptimal gut microbes
- Promotes a healthy and balanced inflammatory response
- Supports healthy blood sugar control
You can find a fantastic source of L. plantarum in Probiotic Breakthrough. Pairing it with Microbiome Breakthrough will give you just what you need to support a healthy gut barrier and flora. Biome breakthrough contains synbiotics (a blend of probiotics and prebiotics) to make probiotics even more effective. IgYmax in Microbiome Breakthrough can safely and specifically bind suboptimal microbes and escort them out of your gut.
Plant Fiber And Polyphenols
Increasing your plant fiber intake and polyphenols is a great way to feed good bacteria and decrease inflammation.
In a study of 10 healthy fasting subjects, participants ate a high-fat, high-calorie meal either with or without 30g of insoluble fiber. While those who ate the meal alone experienced an increase in LPS, those who ate the additional fiber did not experience an increase in LPS. Therefore, adding fiber to your diet can help keep your gut healthy by maintaining low LPS levels and preventing the inflammatory effects of a high-fat diet.
Eating a diet high in polyphenols has similar effects to dietary fiber. When ten healthy subjects consumed grape polyphenols along with a high-fat meal, it prevented oxidative stress and increased LPS compared to the placebo group. This highlights the anti-inflammatory and antioxidant benefits of adding polyphenols to your diet.
Plant fibers and polyphenols also play an important role in increasing the good bacteria in your gut. Both serve as prebiotics for your good gut bacteria to stimulate their growth and help maintain the proper balance in your gut.
One way to ensure you’re getting enough fiber and polyphenols in your diet is to focus on a plant-based diet or simply eat more plants.
Omega-3 Fatty Acids
In contrast to the pro-inflammatory nature of saturated and omega-6 fats, increasing your unsaturated fat intake helps with metabolic endotoxemia. Omega-3 fatty acids promote a balanced inflammatory response by helping regulate the diversity and abundance of good gut bacteria.
Some sources of healthy Omega-3s include:
- Fish and other seafood (especially fatty fish like mackerel, salmon, and herring)
- Nuts and seeds
- Flaxseed oil
An 8-week placebo-controlled study of 67 individuals explored the effects of Omega-3s on endotoxemia. Participants either received 900 mg or 3,600 mg of fish oil, or a placebo before a low-dose LPS challenge. Participants who took the high dose of fish oil had a lower inflammatory response to LPS than those who took 900 mg or the placebo. Therefore, a high dose of Omega-3s may help mitigate metabolic endotoxemia.
Avoid Alcohol Consumption

Consuming large amounts of alcohol can overwhelm your gut and eventually cause permeability in your gut lining. It does this by disrupting your gut bacteria and causing dysbiosis in your gut.
A study of 97 excessive drinkers compared to 51 non-drinkers explored the relationship between alcohol consumption and endotoxins. LPS levels were much higher for those who drank than those who did not. Those who consumed more drinks in the past 30 days had higher LPS levels.
Drinking here and there won’t destroy your gut, but it’s best to keep it to a minimum.
The Takeaway
If you’re improving your diet and exercising to improve your health, it’s essential to address all the factors affecting your metabolic health. A leaky gut can undermine all of your best intentions. Be proactive and take the following steps:
- Balance your fat intake while eating less salt and sugar
- Increase your omega-3s consumption
- Take a quality probiotic like Probiotic Breakthrough and complement it with Microbiome Breakthrough to heal and protect your gut.
- Increase your fiber and polyphenol intake.
- Keep alcohol consumption to a minimum.
- Talk to your functional health practitioner to have your LPS levels tested if you think metabolic endotoxemia may be an issue for you.
If you’re improving your diet and exercising to improve your health, it’s essential to address all the factors affecting your metabolic health. A leaky gut can undermine all of your best intentions. Be proactive and take the following steps:
References
- Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017;11(9):821-834. doi:10.1080/17474124.2017.1343143
- Bertók L. Bacterial endotoxins and their effects. Orv Hetil. 1998;139(33):1947-1953.
- Harju K, Ojaniemi M, Rounioja S, et al. Expression of toll-like receptor 4 and endotoxin responsiveness in mice during perinatal period. Pediatr Res. 2005;57(5 Pt 1):644-648. doi:10.1203/01.PDR.0000156212.03459.A9
- Ghosh S, Lertwattanarak R, Garduño J de J, et al. Elevated muscle TLR4 expression and metabolic endotoxemia in human aging. J Gerontol A Biol Sci Med Sci. 2015;70(2):232-246. doi:10.1093/gerona/glu067
- Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 2017;13(4):851-863. doi:10.5114/aoms.2016.58928
- Lassenius MI, Pietiläinen KH, Kaartinen K, et al. Bacterial endotoxin activity in human serum is associated with dyslipidemia, insulin resistance, obesity, and chronic inflammation. Diabetes Care. 2011;34(8):1809-1815. doi:10.2337/dc10-2197
- Zhao M, Chen X. Effect of lipopolysaccharides on adipogenic potential and premature senescence of adipocyte progenitors. Am J Physiol Endocrinol Metab. 2015;309(4):E334-44. doi:10.1152/ajpendo.00601.2014
- de La Serre CB, de Lartigue G, Raybould HE. Chronic exposure to low dose bacterial lipopolysaccharide inhibits leptin signaling in vagal afferent neurons. Physiol Behav. 2015;139:188-194. doi:10.1016/j.physbeh.2014.10.032
- Izquierdo AG, Crujeiras AB, Casanueva FF, Carreira MC. Leptin, obesity, and Leptin resistance: Where are we 25 years later? Nutrients. 2019;11(11):2704. doi:10.3390/nu11112704
- Manco M, Putignani L, Bottazzo GF. Gut microbiota, lipopolysaccharides, and innate immunity in the pathogenesis of obesity and cardiovascular risk. Endocr Rev. 2010;31(6):817-844. doi:10.1210/er.2009-0030
- Liang H, Hussey SE, Sanchez-Avila A, Tantiwong P, Musi N. Effect of lipopolysaccharide on inflammation and insulin action in human muscle. PLoS One. 2013;8(5):e63983. doi:10.1371/journal.pone.0063983
- Kiechl S, Lorenz E, Reindl M, et al. Toll-like receptor 4 polymorphisms and atherogenesis. N Engl J Med. 2002;347(3):185-192. doi:10.1056/NEJMoa012673
- Wang J, Si Y, Wu C, et al. Lipopolysaccharide promotes lipid accumulation in human adventitial fibroblasts via TLR4-NF-κB pathway. Lipids Health Dis. 2012;11(1):139. doi:10.1186/1476-511X-11-139
- Määttä AM, Salminen A, Pietiäinen M, et al. Endotoxemia is associated with an adverse metabolic profile. Innate Immun. 2021;27(1):3-14. doi:10.1177/1753425920971702
- Wang J, Jia Y, Li G, et al. The dopamine receptor D3 regulates lipopolysaccharide-induced depressive-like behavior in mice. Int J Neuropsychopharmacol. 2018;21(5):448-460. doi:10.1093/ijnp/pyy005
- Lasselin J, Lekander M, Benson S, Schedlowski M, Engler H. Sick for science: experimental endotoxemia as a translational tool to develop and test new therapies for inflammation-associated depression. Mol Psychiatry. 2021;26(8):3672-3683. doi:10.1038/s41380-020-00869-2
- Zhan X, Stamova B, Sharp FR. Lipopolysaccharide associates with amyloid plaques, neurons and oligodendrocytes in Alzheimer’s disease brain: A review. Front Aging Neurosci. 2018;10:42. doi:10.3389/fnagi.2018.00042
- Cani PD, Amar J, Iglesias MA, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56(7):1761-1772. doi:10.2337/db06-1491
- Rohr MW, Narasimhulu CA, Rudeski-Rohr TA, Parthasarathy S. Negative effects of a high-fat diet on intestinal permeability: A review. Adv Nutr. 2020;11(1):77-91. doi:10.1093/advances/nmz061
- Ghanim H, Abuaysheh S, Sia CL, et al. Increase in plasma endotoxin concentrations and the expression of Toll-like receptors and suppressor of cytokine signaling-3 in mononuclear cells after a high-fat, high-carbohydrate meal: implications for insulin resistance. Diabetes Care. 2009;32(12):2281-2287. doi:10.2337/dc09-0979
- Deopurkar R, Ghanim H, Friedman J, et al. Differential effects of cream, glucose, and orange juice on inflammation, endotoxin, and the expression of Toll-like receptor-4 and suppressor of cytokine signaling-3. Diabetes Care. 2010;33(5):991-997. doi:10.2337/dc09-1630
- Wang C, Huang Z, Yu K, et al. High-salt diet has a certain impact on protein digestion and gut Microbiota: A sequencing and proteome combined study. Front Microbiol. 2017;8:1838. doi:10.3389/fmicb.2017.01838
- Ferguson JF, Aden LA, Barbaro NR, et al. High dietary salt-induced dendritic cell activation underlies microbial dysbiosis-associated hypertension. JCI Insight. 2019;5(13). doi:10.1172/jci.insight.126241
- Garcia K, Ferreira G, Reis F, Viana S. Impact of dietary sugars on gut Microbiota and metabolic health. Diabetology. 2022;3(4):549-560. doi:10.3390/diabetology3040042
- Sánchez-Tapia M, Martínez-Medina J, Tovar AR, Torres N. Natural and artificial sweeteners and high fat diet modify differential taste receptors, insulin, and TLR4-mediated inflammatory pathways in adipose tissues of rats. Nutrients. 2019;11(4):880. doi:10.3390/nu11040880
- Rackerby B, Kim HJ, Dallas DC, Park SH. Understanding the effects of dietary components on the gut microbiome and human health. Food Sci Biotechnol. 2020;29(11):1463-1474. doi:10.1007/s10068-020-00811-w
- Kumar Singh A, Cabral C, Kumar R, et al. Beneficial effects of dietary polyphenols on gut Microbiota and strategies to improve delivery efficiency. Nutrients. 2019;11(9):2216. doi:10.3390/nu11092216
- Ojo O, Ojo OO, Zand N, Wang X. The effect of dietary fibre on gut Microbiota, lipid profile, and inflammatory markers in patients with type 2 diabetes: A systematic review and meta-analysis of randomised controlled trials. Nutrients. 2021;13(6):1805. doi:10.3390/nu13061805
- Alves-Santos AM, Sugizaki CSA, Lima GC, Naves MMV. Prebiotic effect of dietary polyphenols: A systematic review. J Funct Foods. 2020;74(104169):104169. doi:10.1016/j.jff.2020.104169
- Moludi J, Kafil HS, Qaisar SA, Gholizadeh P, Alizadeh M, Vayghyan HJ. Effect of probiotic supplementation along with calorie restriction on metabolic endotoxemia, and inflammation markers in coronary artery disease patients: a double blind placebo controlled randomized clinical trial. Nutr J. 2021;20(1):47. doi:10.1186/s12937-021-00703-7
- Lee SJ, Bose S, Seo JG, Chung WS, Lim CY, Kim H. The effects of co-administration of probiotics with herbal medicine on obesity, metabolic endotoxemia and dysbiosis: a randomized double-blind controlled clinical trial. Clin Nutr. 2014;33(6):973-981. doi:10.1016/j.clnu.2013.12.006
- Rouxinol-Dias AL, Pinto AR, Janeiro C, et al. Probiotics for the control of obesity – Its effect on weight change. Porto Biomed J. 2016;1(1):12-24. doi:10.1016/j.pbj.2016.03.005
- Fidanza M, Panigrahi P, Kollmann TR. Lactiplantibacillus plantarum-nomad and ideal probiotic. Front Microbiol. 2021;12:712236. doi:10.3389/fmicb.2021.712236
- Bomba A, Nemcová R, Mudroňová D, Guba P. The possibilities of potentiating the efficacy of probiotics. Trends Food Sci Technol. 2002;13(4):121-126. doi:10.1016/s0924-2244(02)00129-2
- Ghanim H, Batra M, Abuaysheh S, et al. Antiinflammatory and ROS suppressive effects of the addition of fiber to a high-fat high-calorie meal. J Clin Endocrinol Metab. 2017;102(3):858-869. doi:10.1210/jc.2016-2669
- Ghanim H, Sia CL, Korzeniewski K, et al. A resveratrol and polyphenol preparation suppresses oxidative and inflammatory stress response to a high-fat, high-carbohydrate meal. J Clin Endocrinol Metab. 2011;96(5):1409-1414. doi:10.1210/jc.2010-1812
- Kumar M, Pal N, Sharma P, et al. Omega-3 fatty acids and their interaction with the gut microbiome in the prevention and amelioration of type-2 diabetes. Nutrients. 2022;14(9):1723. doi:10.3390/nu14091723
- Ferguson JF, Mulvey CK, Patel PN, et al. Omega-3 PUFA supplementation and the response to evoked endotoxemia in healthy volunteers. Mol Nutr Food Res. 2014;58(3):601-613. doi:10.1002/mnfr.201300368
- Mutlu EA, Gillevet PM, Rangwala H, et al. Colonic microbiome is altered in alcoholism. Am J Physiol Gastrointest Liver Physiol. 2012;302(9):G966-78. doi:10.1152/ajpgi.00380.2011
- Liangpunsakul S, Toh E, Ross RA, et al. Quantity of alcohol drinking positively correlates with serum levels of endotoxin and markers of monocyte activation. Sci Rep. 2017;7(1):4462. doi:10.1038/s41598-017-04669-7